
The Importance Of Radiology In Cancer Care And The Multidisciplinary Team Approach
It is said that radiology often serves as the patient entry point into the cancer care system (Weldon, 2016). As part of a thorough assessment, imaging studies are often included to differentiate potential diagnoses. Imaging plays an integral role throughout the cancer care continuum; aiding with the initial diagnosis, treatment monitoring, and surveillance. At Veterans Affairs Long Beach Healthcare System (VALBHS), prostate and lung cancers have been the most prevalent diagnoses over the past several years. In 2015, smoking prevalence in the general adult population was approximately 15% in the United States, while that of the veteran population was approximately 16.8% in the same year (U.S. Department of Veterans Affairs). Smoking is a key factor in many disease processes including, but not limited to, multiple types of cancer, COPD, and heart disease.
Cancer care is highly complex and, without care coordination, timely follow-up of abnormal imaging results remains a challenge within specialty clinics. To address these challenges, VALBHS deploys nurse cancer care coordinators (NCCC) in outpatient specialty clinics. Their interdependence is a core principle and is essential to address illnesses specific to military service. The nomenclature may differ throughout healthcare settings; case managers, case coordinators, care managers, or navigators; however, the function remains essentially the same. Irrespective of terminology, these NCCCs have a vital role and responsibility to ensure veterans receive optimal coordination, timely follow-up, and circumvent loss to follow-ups and gaps in service.
VALBHS employs two types of cancer care coordinators: The first manage possible malignancy detected on imaging, while the second coordinates complex cancer cases presented and discussed during tumor boards. Extensive knowledge and rigorous teamwork are imperative in addressing the complexity of cancer coordination across specialty services. NCCCs specialize in radiology and cancer management. They serve as a vital member of the tumor board review team. The multidisciplinary tumor board includes a cancer care coordinator, oncologist, radiation oncologist, surgeon, pathologist, and radiologist. The two roles of the NCCC ensure that the plan of care developed during the tumor board is accurately documented and discussed with the veteran to guarantee a patient-centered plan is executed. Both roles are essential in providing quality and ensuring that the veteran’s values drive decision-making throughout the cancer care continuum.
RADIOLOGY IN CANCER MANAGEMENT
In 2019, approximately 5,000 out of 100,000 imaging tests completed at VALBHS resulted in “possible malignancy” findings, and ultimately 600 newly diagnosed malignancies. Managing a possible malignancy is labor-intensive; however, it is essential to ensure timely workup and improved outcomes. A delayed cancer diagnosis is the most common reason for ambulatory malpractice claims and is associated with increased anxiety and poor outcomes (Murphy 2015).
The VALBHS has multiple onsite imaging resources aimed at providing seamless care. These advanced imaging technologies include CT, MRI, PET, bone scan, interventional radiology guided biopsy, cryoablation, radiofrequency ablation, and stereotactic radiation. When image results are reviewed, and an abnormal finding is identified, a code alert is entered into the electronic medical record. Fragmentation of care in the outpatient setting can impede the timely follow-up of abnormal diagnostic imaging. Evidence demonstrates the critical imaging results may not receive timely follow-up even when healthcare providers receive and read results in an electronic medical record system (Singh, 2009). A multidisciplinary approach including engaged care coordinators is needed to improve patient safety and expedite care and treatment for patients with cancer.
This code alert mechanism utilized at the VALBHS system sends an automated notification of possible malignancy to the lead care coordinator in specialty clinics, the ordering provider, and the primary care provider. The lead care coordinator is a Certified Case Manager who acts as a supervisor for our outpatient specialty clinics and inpatient case management. This nurse has extensive knowledge and expertise in reviewing abnormal alerts, ensures follow up by the appropriate service, and acts as a safety net for our facility. The lead care coordinator reviews the urgency of the alert and assigns the case to the NCCC. VALBHS utilizes a care management tool, a web-based application that facilitates team-based, patient-related task management and tracking. This tool was created to eliminate the disparate approaches that were utilized by care coordinators.
Initial imaging studies are performed to evaluate a specified complaint or condition. Occasionally incidental findings are captured that may require additional imaging or follow-up. An example of incidental finding: A veteran comes to the orthopedic clinic for lower back pain, and an MRI of the L-spine is ordered. A finding of possible renal cell carcinoma is found, triggering additional imaging and surgical urology consult for further evaluation. The NCCC follows up on incidental findings in specialty care. NCCC is an extremely important role to ensure effective and high-quality medical care is delivered. Imaging is involved throughout the continuum of cancer care to help detect, stage, as well as monitor the progression of the disease.
MULTIDISCIPLINARY APPROACH
The mean and median age of veterans with cancer at VALBHS is approximately 67 years old. A new cancer diagnosis adds another layer to the medical complexity within this population. Veterans of this age group often have compounded chronic medical, psychiatric, and psychosocial issues complicating their plan of care. The NCCC is essential in navigating the care throughout the continuum in this complex population. Healthcare, in general, tends to work in silos, along with inconsistent communication that can result in care delays, decreased patient satisfaction, and fragmentation of care. Initiating a multidisciplinary team at the onset of diagnosis assists in eliminating these barriers (Weldon, 2016).
VALBHS has a comprehensive approach to providing cancer care through multidisciplinary tumor boards. Tumor boards consist of an NCCC, pathologist, radiologist, oncologist, radiation oncologist, surgeon, and other specialists as needed. Thoracic, urology, general, neuro-oncology as well as liver tumor boards meet weekly or biweekly to discuss complicated cases and determine the best course of action for veterans with cancer. These long-standing tumor boards have fostered a cohesive relationship between providers and streamlined communication and processes, thus decreasing fragmented care. Other benefits of this forum are to provide consensus on evidence-based care for an individual patient and provides an avenue for discussing clinical trials, as well as specifically targeted immunotherapies. Multidisciplinary programs have proven to be successful in increasing patient satisfaction and shortening the time between diagnosis and treatment (Parman, 2018).
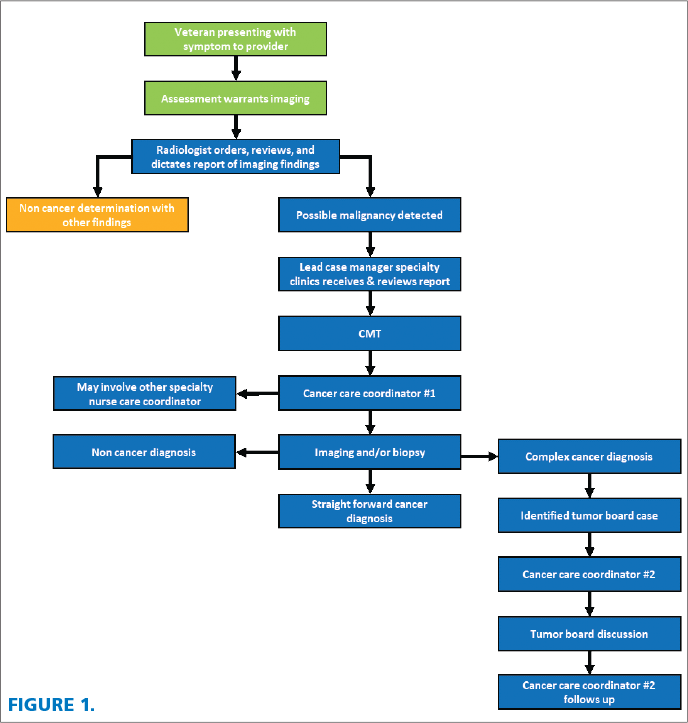
The role of the NCCC is vital to the multidisciplinary tumor board so that the multidisciplinary plan is communicated and the veteran is driving their own care. They serve as the key point of contact for all the disciplines and the veteran. Closed-loop communication becomes essential to ensure that care delivery is received, acknowledged, and acted upon in a timely manner (Lee, et al). The NCCC provides an invaluable service in expediting workup and treatment for some of the most complex cancer cases. See figure 1 for the flow chart of the veteran cancer care process as it generally occurs.
The case study presented below highlights the work of nurse cancer care coordinators within the multidisciplinary team.
CASE STUDY
A 63-year-old male veteran presents to the emergency room with stroke-like symptoms. He has a history of smoking, coronary artery disease, type 2 diabetes, HTN, hyperlipidemia, and peripheral arterial disease. Several CT scans are completed including a CT angiogram neck, which demonstrates the expected findings of occlusion in a carotid artery. However, the CTA incidentally shows a spiculated lesion in the lung apex.
The veteran is seen by a neurologist with recommendations for interventional radiology versus neurosurgery to evaluate for stent versus endarterectomy. A higher level of care is needed for this procedure, and he is transferred to the community hospital, where care is delivered for the next several days. A stent is placed, and further imaging is done. He is placed on blood thinners and cholesterol medication.
The lead case manager receives the possible malignancy alert from the CTA and places the veteran on the care management tool so that he can be reviewed in pulmonary radiology chest conference (PRCC) where a dedicated CT thorax is recommended and ordered. The veteran’s care is coordinated with him, his wife, and Care in the Community office to ensure pertinent imaging is completed at the community hospital where the veteran is receiving care for stent placement. This ensures that the veteran will not have to repeat the imaging, which eliminates additional radiation exposure and cost. After images are obtained from the community hospital, PRCC convenes to review and determine further recommendations that include a PET scan for cancer staging and consult for interventional radiology for a possible biopsy. The cancer care coordinator coordinates with neurology, pulmonary, and radiology.
The stent placement for CVA management and workup for lung cancer occurred during COVID-19, necessitating testing before the biopsy and additional care coordination during a pandemic. Once the biopsy is completed, the pathology report shows a squamous cell carcinoma in the right upper lobe of the lung. The PET scan shows hilar hypermetabolism but is unclear if this is inflammation versus malignancy. The veteran care is discussed in the thoracic tumor board in which the NCCC arranges for neurology and a neuroradiologist to attend due to recent stent placement for CVA to ensure a holistic plan incorporating all risks and comorbidity in his plan of care.
The recommendation of the multidisciplinary team is to repeat the biopsy to determine if there was a metastatic lesion or second primary lung cancer. There is a robust discussion regarding performing endobronchial ultrasound (EBUS) by pulmonary to obtain a biopsy or having thoracic surgery do mediastinoscopy and possible lobectomy. The veteran would also need pulmonary function tests and another swab for COVID-19 as well as to be cleared by anesthesiology for general anesthetic before the second biopsy. More imaging is ordered, and formal evaluations by oncology, radiation, and anesthesia are needed.
The NCCC is an integral part of ensuring all studies and consults are coordinated expeditiously. This case was discussed multiple times in the thoracic tumor board to discuss new findings. The final consensus is that the veteran is not felt to be a good candidate for lung resection or EBUS due to severe cardiovascular disease and the location of the lesion. The veteran is part of shared decision making to proceed with chemo and/or radiation and then reimage within three months. The NCCC plays an essential role in all tumor board discussions, validates, and executes the care plan in agreement with the veteran and his family.
CONCLUSION
The VA Long Beach Healthcare System has a long history of caring for veterans with cancer. As cancer becomes more complex and the survival rate is improved, veterans’ conditions are managed as a chronic illness in the Survivorship Clinic. Radiology is a vital component of cancer care management throughout the continuum. The NCCC is essential in expediting time from diagnosis to treatment as well as providing quality cancer care and improved outcomes.
Multidisciplinary tumor boards ensure communication and collaboration for cases that have a higher level of complexity and require input from specialty care providers. NCCCs play a key role in tumor boards to ensure that the plan of care in motion continues, that the veteran and family are supported, resources are provided, and silos are eliminated during their cancer journey. Coordinating care is an essential component of providing veteran-centric care for our nation’s finest.
REFERENCES
Lee, S., Clark, M., Cox, J., Needles, B., Seigel, C., & Balasubramanian, B. (2016). Achieving coordinated care for patients with complex cases of cancer: A multiteam system approach. American Society of Clinical Oncology, 12(11), 1029-1038. doi:10.1200/JOP.2016.013664
Murphy, D., Louis Wu, E., Forjuoh, S., Meyer, A., & Singh, H. (2015) Electronic Trigger Based Intervention to Reduce Delays in Diagnostic Evaluation for Cancer: A Cluster Randomized Controlled Trial. Journal of Clinical Oncology 33
Parman, Cindy, (2018) Compliance Multidisciplinary Clinic Visits, https://www.accc-cancer.org/docs/documents/oncologyissues/articles/so18/compliance.pdf?sfvrsn=5423a19_11
Singh, H., Thomas, E., Shrinidi, M., Sittig, D., Harvinder, A., Espadas, D., Khan, M., & Petersen, L., (2009) Timely Follow-up of Abnormal Diagnostic Imaging Test Results in an Outpatient Setting. Archives of Internal Medicine 169(17) 1578-1586
VHA Office of Quality, Safety and Value. (2016). Care Management Tool. Retrieved from https://dvagov.sharepoint.com/sites/vhacare-management-tool-cmt/Shared%20Documents/Forms/AllItems.aspx?id=%2Fsites%2Fvhacare%2Dmanagement%2Dtool%2Dcmt%2FShared%20Documents%2FVA%20Product%20Effectiveness%20Evaluation%20%2Epdf&parent=%2Fsites%2Fvhacare%2Dma
Weldon, C. B., Friedewald, S. M., Kulkarni, S. A., Simon, M. A., Carlos, R. C., Strauss, J. B., … Trosman, J. R. (2016). Radiology as the point of cancer patient and care team engagement: Applying the 4R model at a patient’s breast cancer care initiation. Journal of the American College of Radiology, 13, 1579-1589. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5127438/
Primary Care and Tobacco Cessation Handbook A Resource for Providers VA U.S. Department of Veterans Affairs https://www.mentalhealth.va.gov/quit-tobacco/docs/IB_10-565-Primary-Care-Smoking-Handbook-PROVIDERS-508.pdf#:∼:text=%20%20%20Title%20%20%20Primary%20Care,Created%20Date%20%20%2010%2F4%2F2017%2012%3A33%3A53%20PM%20





