Legislation in Action Dealing with the Opioid Crisis
BY , RN, MSN, MHA, MA, CCM, ACM-RN, CPHM, , RN, BSN, CRRN, CCM, JD, , RN, MSN, AND , MSN, BA, RN-BC
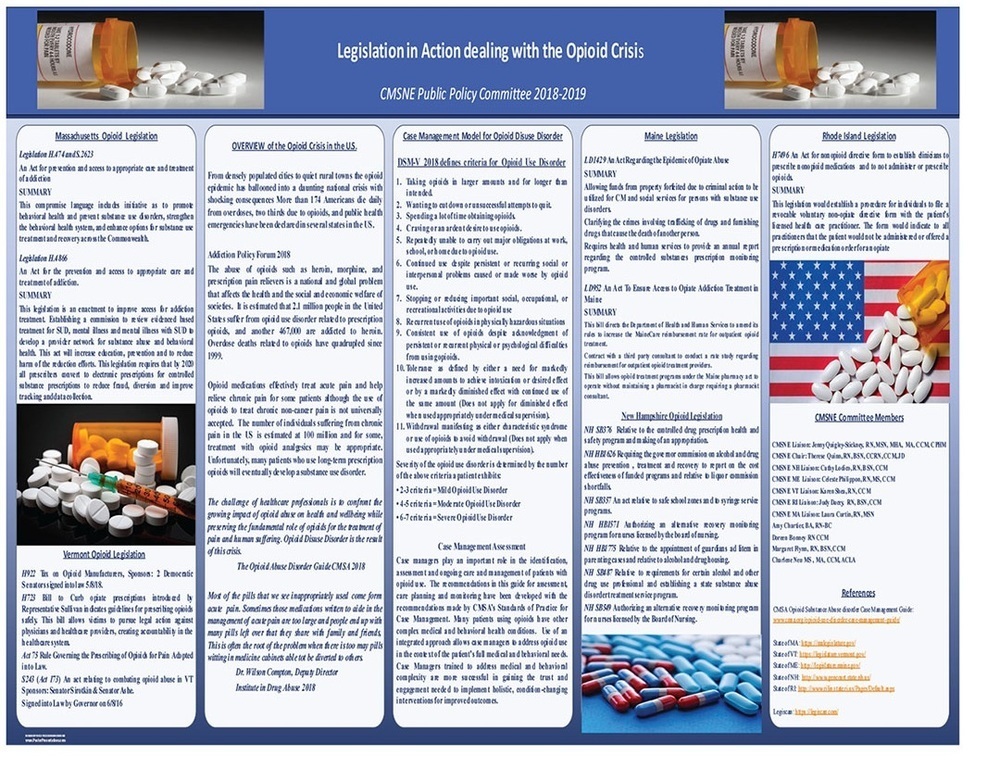
The CMSNE Public Policy Committee developed our 2020 poster entitled “Opioid Legislation in Action for Professional Case Managers” as a follow-up to our 2018-2019 poster, “Legislation in Action Dealing with the Opioid Crisis.” The latter poster was presented at the CMSA Annual Conference in Las Vegas, and it was extremely well-received. The interest, discussions, and feedback prompted the Public Policy Committee to develop a poster discussing some of the programs that were developed as a result of the opioid legislation passed in the New England states.
In our 2018-2019 poster, we provided an overview of the opioid crisis in the United States, including the Opioid Crisis Response Act of 2018, which catapulted legislation on a state level. We outlined legislation that was occurring in the New England states.
In Massachusetts, the focus was on the promotion of behavioral health options for the prevention and treatment of substance use disorders (SUD). This proposed legislation included establishing a commission to review evidence-based treatment for SUD, mental illness, and dual diagnosis (mental illness and SUD) and establish a provider network to manage these conditions. The proposed legislation included a requirement that, by 2020, all prescribers convert to electronic prescriptions for controlled substances in an attempt to reduce fraud and improve tracking and data collection.
In Vermont, the legislation was designed to create accountability on the part of prescribers. Guidelines were enacted to encourage safe prescribing practices for opioids.
The New Hampshire legislation addressed establishing a state-based substance abuse disorder treatment program and a governor commission on alcohol and drug abuse prevention, reviewing efficacy and cost-effectiveness of various programs. The legislation included an alternative recovery monitoring program for nurses licensed by the NH Board of Nursing and appointment of guardians ad litem in parenting cases and relative to housing.
In Maine, there was a bill directing the Department of Health and Human Services to amend rules to increase the MaineCare reimbursement rate for outpatient opioid treatment. There was legislation to allow funds seized from property forfeited as a result of criminal action to be utilized for case management and social services for persons with SUD.
Rhode Island’s legislation focused on establishing a procedure for individuals to file a revocable voluntary non-opiate directive form with his/her healthcare practitioner to indicate that opioid prescriptions would not be offered to that individual.
We provided the DSM-V definition and criteria for opioid disuse disorder and discussed the role of the professional case manager in identifying, assessing, and managing the complex care of individuals with regard to opioid use in accordance with the CMSA Standards of Practice for Case Management.
In 2018, the CMSNE Public Policy committee began a project examining the opioid disuse disorder and its impact on the New England states, patient care, and communities that professional case managers serve. Each member of the public policy committee researched current legislation proposed and passed within the CMSNE Chapter Five state region. This research was then combined into a multistate group project and poster submission for the 2019 CMSA annual conference in Las Vegas. The first poster presentation highlighted the 2018 Federal Opioid Act and followed legislation that mirrored this legislation or legislation within each New England state that provided resources specific to the states’ needs for controlling and managing the opioid disuse disorder.
The Opioid Crisis Response Act is one of the first federal interagency legislation passed in 2018 that provided comprehensive opioid prevention, education, treatment, monitoring of controlled substances, support for patients and families, awareness of social determinants of health that impact recovery, access to care through proposed telehealth models for recovery, data collection and technology for drug monitoring and prescription (PDMP information) available to states through shared technology while maintaining confidentiality to provide effective evidenced-based treatment programs.
The second poster, “Opioid Legislation in Action for the Professional Case Manager,” examined the actual resources created by this legislation and evidence-based practice resources available in 2019 for professional case managers to utilize within the five New England communities they serve.
Due to changes from the COVID-19 pandemic, the second poster was presented in an entirely new format. The 2020 CMSA Annual Conference was transitioned to a virtual platform utilizing the learning toolbox for the poster presentations, which allowed the poster to not only be presented online but also to be accessed through online links to all five of the states’ legislative sites to view legislation supporting opioid use disorder resources in each state.
Massachusetts led the evolution of opioid resources for case managers and created House Bill 4742, the “CARE Act,” which mirrored federal legislation. This legislation expanded the existing Step Act program in Massachusetts, which provided preventative care, treatment programs, limited opioid prescribing practices, and allocated educational funding dedicated to the risks associated with opioid misuse. The CARE Act revised Massachusetts’ anti-kickback statute to prohibit manufacturers from offering any discount, rebate, product voucher, or other reduction in an individual’s out-of-pocket expenses, including co-payments and deductibles, for any Schedule II opioid. For purposes of this rule, Schedule II opioids include any substance having an addiction-forming or addiction-sustaining liability similar to morphine or being capable of conversion into a drug having addiction-forming or addiction-sustaining liability. The CARE Act includes a number of provisions that affect healthcare providers’ practices and autonomy, such as increased access to naloxone (the opioid overdose reversal drug), liability protection for prescribers of opioids, expanded scope of practice for prescribers, expanded access to partial fills, mandatory electronic prescribing, workers’ compensation formulary, and prescribing commissions.
The CARE Act in Massachusetts has focused on the expansion of access to Medication Assisted Treatment (MAT) in highly impacted communities and the Department of Corrections, building out access to opioid use disorder (OUD) treatment services. The definition of a licensed mental health professional is expanded in EDs, increasing the number of professionals available to perform substance use disorder evaluations (now includes interns, addiction RNs, and certified substance abuse social workers). Emergency departments across the state are now mandated to have 24/7 availability to a MAT prescriber and social service professionals to guide harm reduction and treatment options for persons who experience overdose in the community.
Some hospital EDs in Boston have developed bridge clinics to support recovery efforts to individuals actively using opiates. EDs are required to track and report the frequency and location of SUD evaluations for persons with overdoses. This act directs EOHHS to develop and implement a statewide remote consultative service to primary care providers in adult settings (17 years of age) for patients with SUD and pain/chronic pain concerns. In addition, The CARE Act enacts a partial fill opiate prescription if requested, and it expands the availability of intranasal Narcan/opioid agonists in the community. Programs continue to build in the state, and the expansion of access to MAT will hopefully have a significant impact on the devastation of opioid use disorder.
Rhode Island has several policies in place regarding opioid therapy, including prescription limitations, insurance coverage, and an outlined standard of treatment for patients with substance use disorder. When prescribing opioids, there must be a limit and no more than 20 doses per day and no more than 30 morphine equivalent doses per day. These limits vary for patients receiving hospice or palliative care, children with pain, chronic pain, and those experiencing pain from cancer. The exclusion also includes those patients residing in a nursing home.
Along with restrictions in prescribing opioids, evaluations and treatments for substance use disorders must be standardized and a large database will be maintained to track those receiving inpatient and outpatient SUD therapy. A nationwide tracking system has also been built to monitor who receives opioids, and prescribers are required to view this system before an opioid prescription is given to a patient. Insurance companies are required to cover all medication-assisted therapies, whereas they previously covered only methadone.
The Stewardship Act allows for SUD treatments, prevention, and educational services. Maine has a similar act in place that assists with the funding of SUD treatment, medications, therapy, drug screens, follow-up visits, and more. Similar to this and providing more resources, New Hampshire is funding programs for those incarcerated with SUD, those born exposed, also adding SUD as a qualifying diagnosis to use medical marijuana.
Vermont is also focusing on funding programs for SUD, making them more accessible and increasing their availability. Programs can be found in schools and through all other age ranges, as there is a Care Alliance in place to partner with healthcare providers in ensuring that all Vermonters lead healthy lifestyles. Recovery coaches provide much of this support to individuals suffering from SUD. Recovery coaches are certified individuals who offer consistent, personalized support throughout their treatment and promote accountability.
Each of the New England states evolved different resources to help fight the opioid disuse syndrome, some mirroring the federal legislation and others creating programs for prevention and treatment, but as we continue to work as professional case managers coping with the challenge of this illness, the exciting aspect of this work will be in the future with analyzing the systems and resources that work and establishing evidenced-based care and resources for our profession.




