BY , DNP, RN, CCM, CMAC, CMCN, ACM-RN
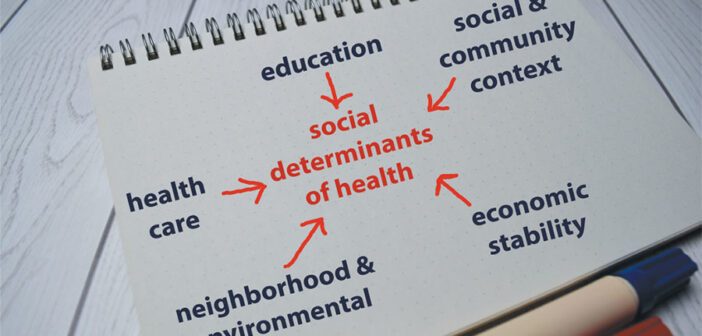
I am honored and excited to be writing the opening to this issue of CMSA Today. The focus for this issue is social determinants of health (SDoH), a subject near and dear to me. SDoH are defined as “life-enhancing resources, such as food supply, housing, economic and social relationships, transportation, education and healthcare, whose distribution across populations effectively determines length and quality of life” (Fink-Samnick, 2018).
“Social determinants of health” is one of the newer buzz phrases in healthcare, but case managers have long known the connection between SDoH and an individual patient’s ability to be successful in managing their health needs. We know that an individual is more than their diagnosis and that healthcare’s failure to create overarching strategies to address the gaps caused by SDoH continues to impact the care continuum’s ability to adequately equip the individual for success in managing their health issues.
We need only take a look at health.gov/healthypeople and the evolution of the program since 1990. In the 1990 version, SDoH were addressed as “reducing food insecurity and hunger” (U.S. Department of Health and Human Services, 2021). The Healthy People 2020 version was the first to formally have a social determinants of health goal: To “create social and physical environments that promote good health for all” (U.S. Department of Health and Human Services, 2021). In the Healthy People 2030 framework, social determinants of health has been broken out into its own topic area with five sub-topics and 113 objectives from creating economic and housing/neighborhood stability, establishing equity in access to healthcare and education, including my “soapbox” of health literacy and developing communities of support.
The impact of SDoH on the healthcare consumer’s ability to self-manage cannot be overstated. According to the American Hospital Association (2018), only 20% of an individual’s health is tied to clinical care, which includes access to and quality of healthcare services. The balance, 80% of an individual’s ability to self-manage BANGOLAND/SHUTTERSTOCK.COM their health needs, is tied to their physical environment, social determinants—where individuals live, work and play—and behavioral factors, including exercise or smoking. More specifically, that 80% can be broken down as follows: 40% is attributed to socio-economic factors, 10% to physical environment and 30% to individual health behaviors.
As you read, review and reflect on the articles this month, I challenge you to consider the following questions related to SDoH:
- How are resources (e.g., food, housing, local businesses, transportation, healthcare services) distributed within your community/practice area?
- How does this compare to surrounding communities?
- What are the relationships between social determinants, cultural and psychological needs and healthcare consumer confidence in self-care?
- What can I/we/my healthcare facility do to address the gaps that our healthcare consumers encounter?
In September of 2020, I was asked to present to the CMSA Fort Wayne Chapter on the topics of “Ethics and Social Determinants of Health.” The participants were incredibly engaged, with lots of great questions, and when I asked that last question of the group, I was thrilled to hear of the community-wide connectivity that Fort Wayne has created to weave a safety net of resources to address the SDoH for their population. So impressed was I that I asked them to consider putting together a presentation for the CMSA National Conference on their program(s) because this is exactly the type of thing we, as case managers, do. We create the solutions to address the needs of our healthcare consumers. We need to get the word out about the great (incredible, crucial) things we do to positively impact individuals, populations and geographic areas.
Consider writing an article, putting together a presentation or poster and let the world know about the work you are doing. You could solve another person’s problem or inspire a new perspective and project.
REFERENCES
American Hospital Association https://www.aha.org/topics/social-determinants-health
Centers for Medicare and Medicaid (2017). Guide to preventing readmissions among racially and ethnically diverse beneficiaries.
Fink-Samnick, E. (2018). Managing the social determinants of health, part I. Professional Case Management, 23(3), 107-129.
Fink-Samnick, E. (2018). Managing the social determinants of health, part II. Professional Case Management, 23(5), 240-255.
Johnson, SR (2018). Complete care. Modern Healthcare, August 27, 2018, 14-18.
Morrison, I (2017). Taking on the social determinants of health. Hospitals and Health Networks, November 2017, p 21-26.
U.S. Department of Health and Human Services. (2021). Healthy People 2030; building a healthier future for all. https://health.gov/healthypeople