Quality improvement and measurement strategies have grown in the United States over the past half century. Although early quality improvement methods originated in the manufacturing industry, healthcare quality improvement methods can be traced back to famous champions in healthcare including Florence Nightingale and Ernest Codman (Marjoua & Bozic, 2012). Notable efforts over the past two decades that have advanced a quality and measurement strategy in the United States include the work by the Institute of Medicine (IOM), The Joint Commission, Centers for Medicare & Medicaid Services (CMS), Agency for Healthcare Research and Quality (AHRQ), National Committee for Quality Assurance (NCQA), National Quality Forum (NQF) and National Quality Strategy (NQS).
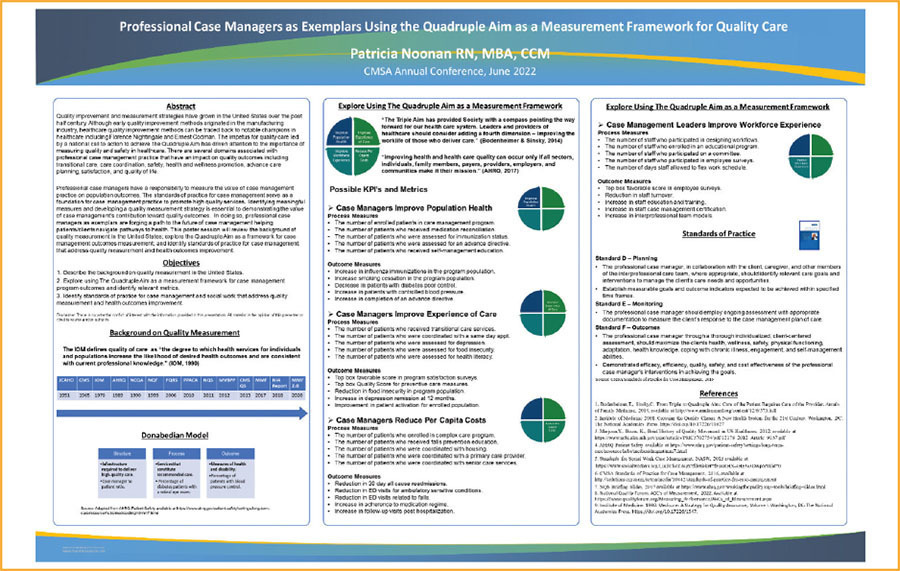
The impetus for quality care led by a national call to action to achieve the Quadruple Aim has driven attention to the importance of measuring quality and safety in healthcare. There are several domains associated with professional case management practice that have an impact on quality outcomes including transitional care, care coordination, safety, health and wellness promotion, advance care planning, satisfaction and quality of life.
THE QUADRUPLE AIM FRAMEWORK
Achieving high-quality healthcare remains an important overarching goal in the United States and throughout the world. What is quality care? The Institute of Medicine (IOM) defined quality of care as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (IOM, 1990). The Triple Aim, introduced by Dr. Berwick and colleagues in 2008, served as a “call to action” for all stakeholders within the healthcare system to work together to improve population health, improve the experience of care and reduce healthcare costs (Bodenheimer & Sinsky, 2014). However, as primary care providers throughout the country sought to achieve the Triple Aim, they quickly recognized a fourth aim was missing, and thus the Quadruple Aim emerged in healthcare. Today, the Quadruple Aim serves as the national clarion for all healthcare providers to achieve: “Leaders and providers of healthcare should consider adding a fourth dimension – improving the worklife of those who deliver care” (Bodenheimer & Sinsky, 2014). Professional case managers working with the healthcare team in all settings across the continuum contribute to the Quadruple Aim by supporting patients/clients, caregivers and providers to achieve patient-centered quality outcomes. In essence, The Quadruple Aim calls for all those who deliver care to improve population health, improve the experience of care, reduce per capita costs and improve the workforce experience.
THE DONEBEDIAN MODEL
In 1966, Dr. Avis Donebedian introduced a standard approach for measuring, evaluating and improving the quality of care to be delivered that included three components: structure, process and outcome (Marjoua & Bozic, 2012). The following example, using the Donebedian Model, is one among hundreds of how the model can be applied to case management program interventions that impact quality care:
Structure: case manager to patient ratio.
Process: percentage of diabetes patients with a retinal eye exam.
Outcome: percentage of patients with blood pressure control.
QUALITY INDICATORS & METRICS
Quality indicators are key performance indicators (KPIs) and metrics that are used by the Centers for Medicare & Medicaid Services (CMS), health plans and other regulatory agencies to measure, report and evaluate the progress made by programs toward the achievement of quality outcomes. The following are examples of possible KPIs and metrics that can be adopted by case managers using the Quadruple Aim Framework as a measurement strategy for quality care:
CASE MANAGERS IMPROVE POPULATION HEALTH
PROCESS MEASURES
- The number of enrolled patients in care management program.
- The number of patients who received medication reconciliation.
- The number of patients who were assessed for immunization status.
- The number of patients who were assessed for an advance directive.
- The number of patients who received self-management education.
OUTCOME MEASURES
- Increase in influenza immunizations in the program population.
- Increase in smoking cessation in the program population.
- Decrease in patients with poor diabetes control.
- Increase in patients with controlled blood pressure.
- Increase in completion of an advance directive.
CASE MANAGERS IMPROVE EXPERIENCE OF CARE
PROCESS MEASURES
- The number of patients who received transitional care services.
- The number of patients who were coordinated with a same-day appointment.
- The number of patients who were assessed for depression.
- The number of patients who were assessed for food insecurity.
- The number of patients who were assessed for health literacy.
OUTCOME MEASURES
- Top box favorable score in program satisfaction surveys.
- Top box quality score for preventive care measures.
- Reduction in food insecurity in program population.
- Increase in depression remission at 12 months.
- Improvement in patient activation for enrolled population.
CASE MANAGERS REDUCE PER CAPITA COSTS
PROCESS MEASURES
- The number of patients enrolled in complex care program.
- The number of patients who received falls prevention education.
- The number of patients who were coordinated with housing.
- The number of patients who were coordinated with a primary care provider.
- The number of patients who were coordinated with senior care services.
OUTCOME MEASURES
- Reduction in 30-day all-cause readmissions.
- Reduction in ED visits for ambulatory sensitive conditions.
- Reduction in ED visits related to falls.
- Increase in adherence to medication regime.
- Increase in follow-up visits post hospitalization.
CASE MANAGEMENT LEADERS IMPROVE WORKFORCE EXPERIENCE
PROCESS MEASURES
- The number of staff who participated in designing workflows.
- The number of staff who enrolled in an educational program.
- The number of staff who participated on a committee.
- The number of staff who participated in employee surveys.
- The number of days staff were allowed to flex work schedules.
OUTCOME MEASURES
- Top box favorable score in employee surveys.
- Reduction in staff turnover.
- Increase in staff education and training.
- Increase in staff case management certification.
- Increase in interprofessional team models.
MEASUREMENT ACCOUNTABILITY
Professional case managers have a responsibility to measure the value of case management practice on population outcomes. The CMSA Standards of Practice for Case Management serves as a foundation for case management practice to promote high-quality services. The following Standards of Practice for Case Management from the CMSA 2016 Standards of Practice highlight the professional case manager’s role in planning, monitoring and outcomes that address the need for measurement.
Standard D – Planning: The professional case manager, in collaboration with the client, caregiver and other members of the interprofessional care team, where appropriate, should identify relevant care goals and interventions to manage the client’s care needs and opportunities.
Establish measurable goals and outcome indicators expected to be achieved within specified time frames.
Standard E – Monitoring: The professional case manager should employ ongoing assessment with appropriate documentation to measure the client’s response to the case management plan of care.
Standard F – Outcomes: The professional case manager, through a thorough individualized, client-centered assessment, should maximize the client’s health, wellness, safety, physical functioning, adaptation, health knowledge, coping with chronic illness, engagement and self-management abilities.
Demonstrate efficacy, efficiency, quality and cost effectiveness of the professional case manager’s interventions (CMSA Standards of Practice for Case Management, 2016).
CASE MANAGERS AS EXEMPLARS PROMOTE QUALITY CARE OUTCOMES
The definition of an exemplar is “one who serves as an ideal model or example” (Merriam-Webster, 2022). Professional case managers as leaders and exemplars are already leading the way to achieve quality care outcomes. However, identifying meaningful measures and developing a quality measurement strategy that includes documenting and reporting program outcomes is essential to demonstrating the value of case management’s contribution toward quality outcomes. Case managers should explore using the Quadruple Aim as a measurement framework for quality care. In doing so, professional case managers as exemplars are forging a path to the future of case management and are demonstrating how they are helping patients/clients navigate pathways to improve their health.
Finally, what does it take to achieve quality healthcare? The Agency for Healthcare Research and Quality stated, “Improving health and healthcare quality can occur only if all sectors, individuals, family members, providers, payors, employers and communities make it their mission” (AHRQ, 2017).
At the core of quality outcomes is the large case management community that is working diligently to drive quality care. Thus, it is imperative that we stake our claim in the quality landscape by raising awareness to senior leaders and policymakers on our contribution toward the Quadruple Aim.
REFERENCES
Bodenheimer, T., Sinsky, C. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Annals of Family Medicine, 2014, available at http://www.annfammed.org/content/12/6/573.full.
Institute of Medicine 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10027.
Marjoua, Y., Bozic, K., Brief History of Quality Movement in US Healthcare, 2012, available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3702754/pdf/12178_2012_Article_9137.pdf.
AHRQ Patient Safety available at https://www.ahrq.gov/patient-safety/settings/long-term-care/resource/hcbs/medicaidmgmt/mm7.html.
Standards for Social Work Case Management, NASW,2013 available at https://www.socialworkers.org/LinkClick.aspx?fileticket=fFnsRHX-4HE%3D&portalid=0.
CMSA Standards of Practice for Case Management, 2016, available at http://solutions.cmsa.org/acton/media/10442/standards-of-practice-for-case-management.
NQS Briefing Slides available at https://www.ahrq.gov/workingforquality/nqs-tools/briefing-slides.html.
National Quality Forum. ABC’s of Measurement, 2022. Available at https://www.qualityforum.org/Measuring_Performance/ABCs_of_Measurement.aspx.
Institute of Medicine. 1990. Medicare: A Strategy for Quality Assurance, Volume I. Washington, DC: The National Academies Press. https://doi.org/10.17226/1547.
.”Exemplar.” Merriam-Webster.com Dictionary, Merriam-Webster, https://www.merriam-webster.com/dictionary/exemplar. Accessed 16 Jun. 2022.
Image credit: SKYLINE GRAPHICS/SHUTTERSTOCK.COM





