
Incorporating Frailty Standards into Case Management
By TIFFANY FERGUSON, LMSW, CMAC, ACM
The Age-Friendly Hospital Rating, introduced as part of the CMS 2025 Inpatient Prospective Payment System (IPPS) Final Rule (HHS, 2024), highlights an opportunity for case managers to play a pivotal role in enhancing care for older adults. The new structural measure is designed to assess hospitals’ commitment to delivering high-quality care to patients aged 65 and older. The rating focuses on five key domains: patient goals, medication management, frailty screening, social vulnerability and leadership commitment. In considering case management assessments, there is a strong opportunity for case managers to significantly contribute to hospital’s compliance and effectiveness in meeting the needs of older patients. Furthermore, the requirements presented in this new standard correlate to the role case managers play across the continuum in supporting older adults.
Understanding the Domains
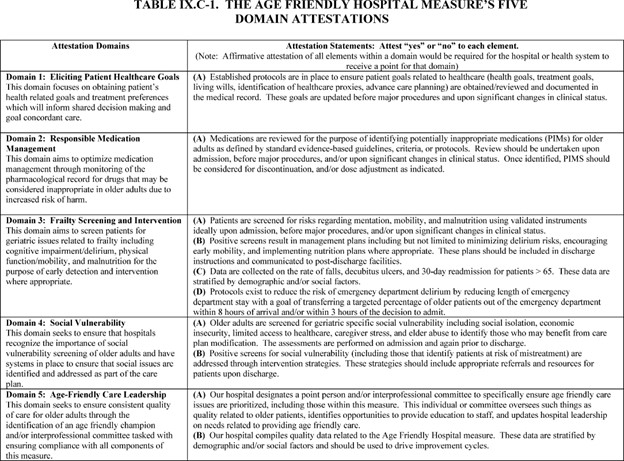
(HHS, 2024)
Eliciting Patient Healthcare Goals: In alignment with the CMSA Standards of Practice (2022), case managers play a crucial role in ensuring a comprehensive understanding of patients’ wishes and interests when developing care plan goals. Through thorough assessment and collaboration, case managers engage in meaningful discussions with older adults and their families to identify care preferences and align treatments with patient-centered objectives. By staying informed about the latest tools and frameworks for shared decision-making, case managers can facilitate these conversations effectively. This approach not only aligns treatment initiatives with patients’ values and priorities but also contributes to improved patient outcomes.
Responsible Medication Management: The emphasis on “responsible” in this standard requires the need for a patient’s clinical care team to go beyond merely maintaining an accurate medication record. It calls for a deeper evaluation of the necessity and interactions of medications in relation to the patient’s overall health and care goals. Achieving this requires enhanced collaboration among patients, pharmacists and providers. Staying current with evidence-based guidelines on polypharmacy and drug interactions, particularly those common in older adults, is crucial. Case managers play a pivotal role by partnering with pharmacists to ensure medication regimens are regularly reviewed and adjusted for safety and efficacy. A comprehensive approach also involves educating patients and their families about medication risks, promoting adherence to prescribed treatments and working with interdisciplinary teams to address medication discrepancies and prevent adverse drug reactions. This coordinated effort supports safer, more effective care for older adults.
Frailty Screening and Intervention: This domain encompasses two key components: completing a comprehensive frailty screening for older adults and developing an individualized intervention strategy. In the acute care setting, this process involves collaboration between nursing, case management and physical and occupational therapy. Similar strategies can also be applied in ambulatory settings.
Case managers are integral in implementing comprehensive frailty assessments by coordinating screenings for malnutrition, mobility challenges and cognitive decline, particularly upon hospital admission, before major surgery, or when planning for safe home management. Familiarity with validated screening tools and interventions is essential to creating effective management plans for at-risk patients. A proactive case management approach, as recommended by Nursing Times (2017), emphasizes the importance of using Comprehensive Geriatric Assessments (CGAs) to develop personalized care plans. CGAs provide a holistic understanding of an older adult’s medical, psychological and social needs. Following the CGA, case managers should work closely with interdisciplinary teams to implement tailored care interventions that support recovery and reduce the risk of adverse outcomes, such as functional decline or hospital readmission. For example, interventions like strength and balance training or nutritional support can effectively address identified risks.
Social Vulnerability: Older adults often face challenges such as social isolation, financial difficulties and inadequate support systems. Case managers can integrate social vulnerability questions into their assessment process to identify these barriers and connect patients with community resources, social services and support networks. Developing a directory of local resources and maintaining strong relationships with community organizations can significantly enhance the ability to address social determinants of health. Additionally, case managers can help facilitate access to services such as transportation, meal delivery programs and housing support ensuring that comprehensive, supportive resources are incorporated into the care planning process. This approach promotes a holistic model of care that addresses both medical and social needs.
Age-Friendly Care Leadership: This domain is a commitment of leadership to advocating for age-friendly practices. The CMSA Standards of Practice (2022) for advocacy and cultural competency demonstrate the case manager’s role to consider and support the impact of the aging adult’s experience in care delivery. On a macro level, case managers can participate in policy development and strategic planning sessions to embed age-friendly principles in the institution’s culture and operational goals.
Criticism of Case Management and Opportunities for Improvement
There has been criticism regarding the impact of case management on improving outcomes related to mortality and reducing the cost of care. A meta-analysis and comprehensive multiyear study published in the Cochrane Review by Sadler et al. (2023), funded by the National Institute of Health, was particularly critical of case management practices. However, a key finding of the research was that the correlation between case managers and improved outcomes in older adults was not necessarily tied to the training or competency of the case managers themselves. The assessment found that while case management for the integrated care of older adults with frailty in community settings was common, the evidence regarding its effectiveness in improving patient outcomes or reducing costs remains uncertain. The review highlighted the need for further research to identify the active components of successful interventions and to understand which patient groups benefit most.
Despite the study’s critical tone, it underscores the necessity for greater research and ongoing evaluation within the field. By regularly assessing case management outcomes, the profession can refine its strategies and enhance its impact. The study also revealed a gap in tailored interventions, emphasizing the need for case managers to design approaches that address the specific needs of older adults, especially those with frailty. This involves customizing care plans based on individual health profiles, preferences and social contexts to ensure a more effective, patient-centered approach.
Promoting Transparency and Quality Improvement
The Age-Friendly Hospital Rating (HHS, 2024) emphasizes the importance of transparent reporting and continuous quality improvement. Case managers’ insights can drive process enhancements to demonstrate our vital role in supporting aging adults. This can include identifying gaps in care delivery through detailed reviews of patient outcomes. For instance, analyzing trends in functional decline or unmet social needs which can inform targeted interventions (Sadler et. al, 2023). Case managers can suggest interventions based on patterns observed in case management activities. For example, increasing access to physical therapy for patients with mobility challenges may address a recurring issue. Professional case managers have a responsibility to engage in performance improvement initiatives aimed at optimizing care for older adult (CMSA, 2022). Participating in age-friendly hospital collaboratives or benchmarking against peer institutions can provide valuable insights and foster innovation.
Alternatively, the Nursing Times (2017) discusses the role of proactive case management, as a cornerstone of effective care for older adults. After conducting a CGA, case managers can work collaboratively with interdisciplinary teams to ensure the seamless implementation of personalized care plans. This includes anticipating patient needs, by identifying potential complications such as hazards and mobility challenges that can be implemented to prevent falls. The article discusses the role of ensuring a smooth transfer between acute, post-acute and community-based care settings, which is a known risk factor for where medication errors and treatment gaps occur, leading to rehospitalization. Applying the Age-Friendly domain for considering the “responsible” portion of medication reconciliation. Finally, the article stresses educating older adults and their families in self-management strategies and available resources to enhance their confidence and autonomy.
The Age-Friendly Hospital measure aims to ensure transparency and consistency in hospital reporting, allowing CMS to monitor and improve the quality of care delivered to older adults across the healthcare system. By challenging our profession to incorporate frailty assessment and age-friendly standards, case managers can be at the forefront of delivering high-quality, age-friendly care. Their efforts not only support hospitals in meeting CMS requirements but also enhance the overall well-being of older adults navigating the healthcare system.
References
Case Management Society of America (CMSA) Standards of Practice for Case Management, Revised 2022.
Department of Health and Human Services (HHS) & Centers for Medicare & Medicaid Services (CMS) August 28, 2024, 42 CFR Parts 405, 412, 413, 431, 482, 485, 495, and 512. CMS-1808-F RIN 0938-AV34. Medicare and Medicaid Programs and the Children’s Health Insurance Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2025 Rates; Quality Programs Requirements; and Other Policy Changes.
Nursing Times, May 22, 2017. Use of proactive case management to address frailty in older people. Retrieved on December 20, 2024 from https://www.nursingtimes.net/older-peoples-nursing/use-of-proactive-case-management-to-address-frailty-in-older-people-22-05-2017/#:~:text=After%20a%20CGA%20has%20been,Health%2C%202010;%202004).
Sadler E, Khadjesari Z, Ziemann A, Sheehan KJ, Whitney J, Wilson D, Bakolis I, Sevdalis N, Sandall J, Soukup T, Corbett T, Gonçalves-Bradley DC, Walker DM. Case management for integrated care of older people with frailty in community settings. Cochrane Database Syst Rev. 2023 May 23;5(5):CD013088. doi: 10.1002/14651858.CD013088.pub2. PMID: 37218645; PMCID: PMC10204122.
 Tiffany Ferguson, MSW, ACM, CMAC, is CEO of Phoenix Medical Management, Inc. Tiffany serves as an adjunct professor at Northern Arizona University, Department of Social Work, and on the American College of Physician Advisors (ACPA) Observation Committee. Tiffany is co-author of The Hospital Guide to Contemporary Case Management through HcPro. She is a contributor for RACmonitor and Case Management Monthly; she also serves on the editorial board for CMSA Today and Care Management. She is a weekly correspondent on SDoH for the news podcast Talk Ten Tuesday. After practicing as a hospital social worker, she went on to serve as director of case management and quickly assumed responsibilities in system level leadership roles in health and care management, which includes CM, UR, CDI, HIM, and coding. She has held C-level responsibility for a large employed medical group, which included value-based arrangements and outpatient care management. Tiffany is a graduate of Northern Arizona University and received her MSW at UCLA.
Tiffany Ferguson, MSW, ACM, CMAC, is CEO of Phoenix Medical Management, Inc. Tiffany serves as an adjunct professor at Northern Arizona University, Department of Social Work, and on the American College of Physician Advisors (ACPA) Observation Committee. Tiffany is co-author of The Hospital Guide to Contemporary Case Management through HcPro. She is a contributor for RACmonitor and Case Management Monthly; she also serves on the editorial board for CMSA Today and Care Management. She is a weekly correspondent on SDoH for the news podcast Talk Ten Tuesday. After practicing as a hospital social worker, she went on to serve as director of case management and quickly assumed responsibilities in system level leadership roles in health and care management, which includes CM, UR, CDI, HIM, and coding. She has held C-level responsibility for a large employed medical group, which included value-based arrangements and outpatient care management. Tiffany is a graduate of Northern Arizona University and received her MSW at UCLA.
Image credit: PAUL MAGUIRE/SHUTTERSTOCK.COM




