
Perspectives On Accountability And Case Management
Accountability and case management come up in many conversations about healthcare quality.
Both are broad terms that have many meanings or implications, especially when they are used together.
To help CMSA Today readers make sense of what can be complex issues, let’s think about how accountability applies to case management.
CASE MANAGERS’ EXPANDING ROLE
The role of case management is growing, a fact that healthcare quality advocates applaud.
The definition of what “counts” as case management is expanding. Physical health, behavioral health, transportation and housing are just some health drivers that can fall under the case management umbrella. Case managers also coordinate services within and between hospitals, health plans, community-based organizations and government agencies. Such diverse duties are why case management may be the most integrated, multidisciplinary role in healthcare today.
The example below of a case involving food insecurity confirms that case management is about more than just healthcare. But first, it helps to consider what accountability can mean to case managers at different levels of the healthcare system.
POPULATION-LEVEL THINKING ABOUT ACCOUNTABILITY
One way to think about quality measurement and accountability is the Applegate model, named for the Ohio Medicaid director who created it.
This model clusters quality measures – and, therefore, opportunities for accountability – at three levels:
- The Macro level includes state and federal regulators.
- The Meso (or middle) level represents organizations that manage care delivery by providers. This level includes accountable care organizations and managed care plans. Organizations at this level respond to regulatory demands from above and consumer needs from below.
- The Micro level represents people and organizations on the front lines, delivering care.
Quality measures and accountability are “nested” and consistent between levels. Goals “cascade down” and quality results “roll up.” In other words, measurement, transparency and accountability are coherent and reinforce each other at all levels.
State governments’ role at the Macro level of the model raises a crucial point: States drive most of the interest in case management.
STATES’ SUPPORT FOR CASE MANAGEMENT AND QUALITY IMPROVEMENT
States are raising the bar to hold community-based organizations accountable for coordinating and managing the care of populations that need long-term services and supports. Affected organizations include Area Agencies on Aging, independent living centers, care management organizations, home and community-based organizations and health plans focused on Managed Medicaid Long-Term Services and Supports.
The American Rescue Plan of 2021 has deepened states’ interest in helping organizations improve quality through effective case management. That legislation, introduced during the pandemic, offered states funding to improve home and community-based services (HCBS) programs.
NCQA Accreditation of Case Management for LTSS is an evidence-based way to assess and improve the care of vulnerable groups, including those served by HCBS programs (https://www.ncqa.org/programs/health-plans/long-term-services-and-supports/). This accreditation is the quality improvement framework 91 organizations have selected to assess and expand accountability (https://reportcards.ncqa.org/other-health-care-organizations?pg=1&filter-program=Case%20Management%20-%20Long-Term%20Services%20and%20Supports).
NCQA Case Management Accreditation (https://www.ncqa.org/programs/health-plans/case-management-cm/) is a related framework that 64 organizations use to apply evidence-based best practices to ensure efficient and cost-effective care (https://reportcards.ncqa.org/other-health-care-organizations?filter-program=Case%20Management&pg=1).
Case managers can modify the NCQA Case Management Accreditation standards into a checklist to assess their own strengths and weaknesses, or those of their organization:
- Program Description: How well does your organization describe your case management services, including the evidence base that supports what you do? Do your responsibilities change based on new evidence?
- Patient Identification and Assessment: How well do you identify patients who qualify for your programs?
- Care Planning: Do you have a process to create individualized care plans?
- Care Monitoring: Do you have systems that support case management activities, monitor individualized care plans and help patients get services they need?
- Care Transitions: Do you have a process to manage transitions of care and identify problems that can result from transitions?
- Measurement and Quality Improvement: Do you measure patient experience, program effectiveness and participation at least once a year?
- Staffing, Training and Verification: Do you plan staffing, organize evidence-based training and check staff credentials?
- Rights and Responsibilities: How well do patients understand what they are entitled to and what is expected of them while they are enrolled in a case management program?
- Delegation of CM: How do you oversee case management responsibilities delegated to other people or organizations?
ACCOUNTABILITY AND CLOSED-LOOP COMMUNICATION
Closed-loop referrals are one way that quality measurement, case management and accountability intersect.
Let’s use food insecurity as an example. A case manager would not only determine that a person lacks reliable access to enough nutritious food – the case manager would be responsible for doing something about it.
Specifically, the case manager might be accountable for what quality measurement professionals call an intermediate outcome: making sure a referral goes to the right food bank or agency that can deal with food insecurity.
(Quality measurement organizations like NCQA feel that case managers should not be responsible for the final outcome – resolving food insecurity is beyond the control of any one person and is hard to track in the long term. But making a timely referral is a specific, measurable and appropriate next step, and it is an opportunity for accountability.)
The figure in the third column illustrates a key point: Accountability is not a “one-and-done” situation. In our example, the case manager who made the referral would contact the receiving agency to confirm and to discuss details. Closing the loop between the sender (case manager) and receiver (food bank) ensures effective care transitions.
In a closed-loop system, the receiver accepts the same level of accountability as the sender. In other words, the receiver confirms “referral received” and loops back to the referring case manager after a meal delivery service is in place.
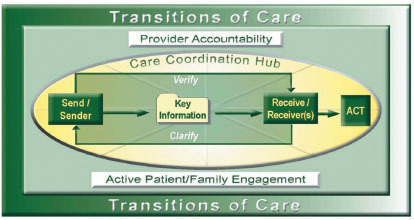
Source: National Transition of Care Coalition, Transition of Care Measures, 2008. Used with permission.
THE BOTTOM LINE
- The care coordination that case managers provide can help correct America’s notoriously fragmented healthcare system. Structured, evidence-based case management can produce coherence and better quality than might otherwise occur.
- Thinking about accountability at various levels of the system can help clarify how case managers at different agencies or organizations connect.
- States increasingly focus on case management as a way to improve care. They use programs such as Case Management Accreditation (https://www.ncqa.org/programs/health-plans/case-management-cm/) and Accreditation of Case Management for Long Term Services and Supports (https://www.ncqa.org/programs/health-plans/long-term-services-and-supports/).
- Quality measurement professionals know and appreciate that effective case management depends largely on a steady cycle of communication, communication and more communication.
Image credit: ISTOCK.COM/DESIGNER491





