
Whole-Person Case Management Practice
Whole-person case management has emerged as an essential practice paradigm in contemporary health systems to address care complexities, fragmentation of services, and widening inequities, and disparities in health outcomes. As the incidence of multiple chronic and complex conditions, behavioral health challenges, and social determinants of health (SDOH) concerns have been increasingly shaping a person’s health and wellbeing outcomes, modern case management models are necessary. Traditional case management practice—focused primarily on resource utilization, care coordination, or discharge and transitional planning—is no longer sufficient to address the multidimensional needs of people and communities. Whole-person case management represents a transformational shift from transactional coordination and utilization management to a deeply relational, integrative, holistic, personal, and equity-oriented approach to care. It reflects the evolving role of the professional case manager as a clinician, advocate, systems navigator, educator, counselor, broker, and partner in a person’s journey toward health and well-being.
This brief article explores whole-person case management practice, highlighting key foundations, recommending a conceptual framework, and delineating related essential professional case manager’s competencies. This practice positions whole-person case management as a central strategy for improving person-centered care, enhancing care quality, advancing health equity, eliminating health disparities, and strengthening population health outcomes. In doing so, the holistic and person-centered model of case management aligns with broader health system reforms including integrated care, value-based payment, health equity initiatives, and interdisciplinary care coordination practices.
Definition of Whole-Person Case Management
Whole-person case management refers to a person-centered, collaborative, and individualized approach to coordinating care across settings and providers, with the person’s values, goals, and lived experience driving every aspect of decision-making and service delivery. It integrates the principles of person-centered care with the professional standards of case management promulgated by the Case Management Society of America (CMSA, 2022) and the code of ethics and professional conduct advanced by the Commission for Case Manager Certification (CCMC, 2025), among other relevant standards. Such integration results in a practice model that honors shared and informed decision-making, respects a person’s autonomy, builds therapeutic partnerships, and ensures continuity of care, for optimal health and wellbeing outcomes for people and communities.
Foundational Values and Principles
Whole-person case management is grounded in several longstanding traditions in nursing, social work, public health, and behavioral and social sciences. At its core is holism, the belief that an individual’s health emerges from the interplay of biological, psychological, cultural, social, behavioral, spiritual, financial, and environmental factors. Although disease-centric thinking is important in care planning and coordination of services, the perspective of whole-person case management positions an individual’s health as a dynamic equilibrium shaped by their life experiences (i.e., SDOH), home environment), identity, structural context, resourcefulness, and personal interests and preferences.
Personhood and dignity are also central to whole-person case management. This principle asserts that every individual possesses inherent worth, autonomy, independence, right to choice, right to refusal, self-determination, and right to be seen. It also honors each person’s individual identity and unique lived experiences. The professional case manager’s role, therefore, is not merely to coordinate services but to build a trusting relationship of mutual respect and empowerment. The person—not the diagnosis—becomes the organizing focus of care planning and coordination of services. Most importantly is having a comprehensive view of the person’s situation, inclusive of the person’s culture, values, belief system, preferences, priority goals, and interests. These are necessary in effectively determining how best to serve, advocate, and advance the person cared for.
Another foundational element is relationship-centered care, which recognizes therapeutic relationships between the professional case manager and recipients of care as essential mechanisms for healing and recovery, trust-building, and active engagement in one’s health and wellbeing. Relationship-centered practice emphasizes presence, active listening, empathy, motivational interviewing, counseling, acceptance, informed decision-making, and shared meaning-making. For professional case managers, effective relationships contribute to comprehensive persons’ assessments and reassessments of needs, personalized care planning, advocacy, and timely coordination of necessary services to meet mutually agreed upon care goals. This is particularly important for individuals experiencing complex and challenging needs.
Cultural humility and respect constitute another cornerstone of whole-person case management. Unlike cultural competence and sensitivity, which risk oversimplifying or stereotyping cultural knowledge and skill, cultural humility emphasizes lifelong self-reflection, recognition of power imbalances, acceptance without judgment, and genuine openness to the individual’s worldview while honoring their diverse beliefs and experiences. This approach aligns with trauma-informed practice, which acknowledges how trauma, discrimination, and systemic inequities influence health behaviors, trust, transparency, and engagement. Therefore, cultural humility is a must have ethical value for the professional case manager. It facilitates building a person’s effective self-management skills, reveals what is not working while sharing the root causes for such concerns in ways that are free of stigma, criticism, or judgment. It also enhances lifestyle behavioral changes with adherence to the personalized health and wellbeing regimens – the plans of care.
Whole-person case management is anchored in equity and social justice. Professional case managers working within this paradigm actively identify and confront structural inequities, advocate for fair access to resources, and work to dismantle barriers rooted in poverty, discrimination, racism, disability status, and other forms of marginalization – SDOHs. This ethical stance distinguishes whole-person case management from traditional models by making equity not an optional consideration but a core clinical responsibility. This approach also helps eradicate the concerns of social determinants of health. Additionally, it assists in ensuring health related social care needs are addressed as a priority and are well integrated into personalized care plans.
Finally, whole-person case management recognizes the importance of strength-based empowerment. This strategy focuses on the intentional practice of professional case managers in recognizing, affirming, and mobilizing a person’s strengths to increase autonomy, confidence, and meaningful participation in shared decision-making regarding own health and wellbeing. This approach to care and care planning also recognizes what already works to build capacity for more ownership; prioritizes what matters most to the person involved to increase their motivation and inspire action; and enhances a person’s resilience while restoring agency in environments of disempowerment they may have previously encountered. Moreover, it is of utmost importance when dealing with a person facing complex chronic conditions or someone who has experienced trauma and social vulnerability.
Conceptual Framework
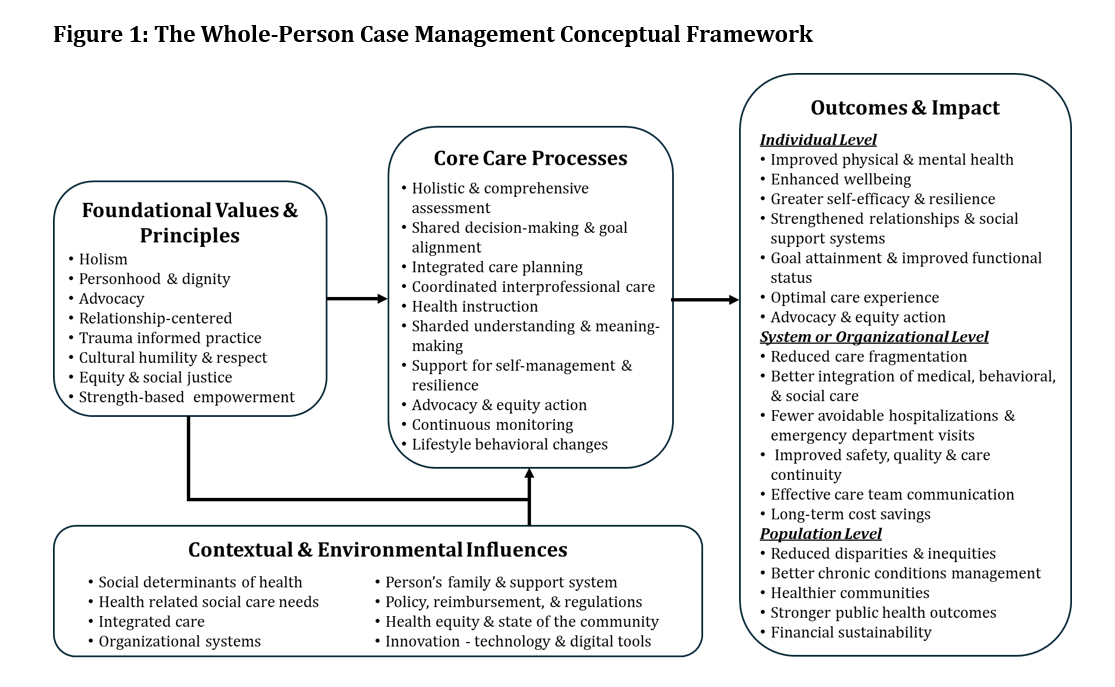
The conceptual framework organizes whole-person case management around four domains: foundational values and principles, core care processes, contextual and environmental influences, and multi-level care outcomes (Figure 1). The values and principles guide the professional case manager’s attitudes, behaviors, and decision-making approaches. They ensure that all interventions remain aligned with what matters most to the person receiving care. They also drive relational and integrative care processes such as holistic assessment, integrated care planning, shared decision-making and goal setting, shared understanding and meaning-making, coordinated interprofessional practice and team-based care, person’s empowerment especially for self-management and lifestyle behavioral adjustment, and most importantly advocacy for equity. Additionally, the values and care processes inform the continuous monitoring of the conditions of those receiving care and adjustment of the intervention, treatments, services, and resources where necessary.
The values and care processes are influenced by contextual and environmental factors related to the systems and recipients of care. These influences emphasize that case management occurs within complex systems that require adaptive, relational, and system’s thinking on an ongoing basis. They comprise four categories:
- Recipients of case management services: chronic health condition, personal support system, SDOHs, HRSNs, innovation in use of technology and digital tools (e.g., artificial intelligence, connected care, and electronic communication systems).
- Community and population health: public health conditions, access to health and social services, security, risk assessment systems, health equity, and health disparities.
- Professional case manager’s practice environment and organizational dynamics: case manager’s competencies, integrated care, quality of care, and safety.
- Sociopolitical environment: regulatory and policy issues, reimbursement methods, value-based care, affordability, and public reporting.
This contemporary conceptual framework illustrates how resources and interventions translate into measurable multi-level outcomes; that is, at the individual, system or organizational, and population or community levels. The whole-person case management framework if implemented effectively must contribute to better clinical, financial, quality, safety, and equity outcomes at all three levels. It also must result in financial stability and sustainability of outcomes which will benefit the recipients of care, the health of the communities served, the livelihood of health care organizations, and the many other stakeholders.
Professional Case Manager Competencies
Essential whole-person case management competencies for professional case managers can be synthesized into seven relevant domains (Figure 2). These support a holistic and comprehensive individual assessment and reassessment of needs, shared and informed decision-making, integrated care planning, interprofessional coordination of services and resources, empowerment for self-management and active engagement in own health, equity-oriented advocacy, and reflective professional practice. Together these competencies prepare professional case managers to operate and practice effectively within complex systems and environments, while maintaining the integrity of whole-person care and services.
The whole-person case management competencies allow professional case managers to ensure care delivery is oriented around integrated systems and processes, interprofessional and team-based approaches, and partnerships across settings and environments. These also facilitate achieving care goals that meet the person’s verbalized preferences and interests while addressing the intertwined dimensions of health and wellbeing. Additionally, the competencies define the required knowledge, skills, attitudes, and behaviors for professional case managers to successfully enact whole-person care with respect, fidelity, and justice.
Conclusion
As health systems have moved toward value-based care and reimbursement models that employ financial risks, person-centered and whole-person case management becomes a necessary model of care. This humanistic model offers a structured, yet adaptable, approach to improving health and wellbeing across individuals, populations, and communities. The synthesis of the whole-person case management framework presented in this article provides professional case managers, case management leaders, and health care executives with a contemporary model for care that ensures achievement of optimal outcomes. The framework integrates the ethical values and principles of case management while emphasizing the interconnectedness of health and human service delivery systems, recognizing the complexity of the systems of care, and positioning the professional case manager at the center of care integration and advocacy for equity and better health outcomes for all.
Health systems embracing whole-person case management framework as described in this article may observe improvements in the recipients of care ability for self-management and engagement in own health; care continuity; quality, safety, and error reduction; equity; and financial outcomes. Given the ongoing transformation toward value-based care, value-based reimbursement, and population health, this framework may serve as a modern interprofessional case management practice model. Additionally, this framework stands as a promising paradigm for improving outcomes across clinical, behavioral, social, and structural dimensions of health.
Figure 1: The Whole-Person Case Management Conceptual Framework
© Copyright 2025, H.M. Tahan, Printed with Permission
Figure 2: Professional Case Managers’ Competencies in Whole-Person Case Management
| Domain | Competency Focus/Highlights |
| 1. Relationship-Centered Communication with the Recipient of Care. |
|
| 2. Holistic & Comprehensive Assessment of the Recipient of Care. |
|
| 3. Shared Decision-Making & Care Planning (with the Recipients of Care and the Interprofessional Care team). |
|
| 4. Care Coordination & Systems Navigation to Ensure Personal Care Goals and Interests Are Met. |
|
| 5. Advocacy, Ethics, Justice, & Equity for the Benefit of the Recipients of Care and Their Support Systems. |
|
| 6. Coaching, Self-Management, & Empowerment of the Recipients of Care to Maintain Health & Wellbeing. |
|
| 7. Professionalism, Leadership, & Reflective Practice to Strengthen Culture of Humility and Eliminate Bias. |
|
© Copyright 2025, H.M. Tahan, Printed with Permission
References
Case Management Society of America (CMSA). (2025). Standards of practice for Case Management. Brentwood, TN: Author.
Commission for Case Management Certification (CCMC). Code of professional conduct for case managers. Mount Laurel, NJ: Author
 Hussein M. Tahan, PhD, RN, FAAN, FCM is a case management expert, consultant, author, professional speaker, and scientist. Hussein is widely published, a co-editor of the CMSA’s Core Curriculum for Case Management, member of the CMSA Today editorial board and advisory board member of the Professional Case Management Journal. Hussein is the recipient of the 2016 CMSA lifetime achievement award and the 2025 National Service Excellence Award.
Hussein M. Tahan, PhD, RN, FAAN, FCM is a case management expert, consultant, author, professional speaker, and scientist. Hussein is widely published, a co-editor of the CMSA’s Core Curriculum for Case Management, member of the CMSA Today editorial board and advisory board member of the Professional Case Management Journal. Hussein is the recipient of the 2016 CMSA lifetime achievement award and the 2025 National Service Excellence Award.




