The COVID-19 pandemic brought about unprecedented change to the U.S. healthcare system, as well as our care management team. It required quick adaptation in order to keep our staff and patients safe, avoid caregiver burnout, maintain job satisfaction and continue to retain our outstanding staff of nurses. Thankfully, the Care Management (CM) Operations department was poised to pivot our workforce to remote positions and, through innovation and technology, continue our work to transition patients and improve the CM work flows through the transition. The CM Operations department consists of both clinical professional staff, utilization management (UM) and clerical teams who support the inpatient CM and UM functions. The clerical or unlicensed teams work under the supervision of a licensed CM. The result of the ongoing Work At Home program at the Cleveland Clinic was increased productivity from our staff, cost savings to the organization and a more satisfied and engaged workforce. This change would not have been possible without the clear standards developed by our management team and the accountability of our staff in maintaining their productivity measures. As a CM leadership team, the emphasis on measuring productivity, proving a financial benefit to the institution and maintaining or improving staff satisfaction was essential to justify the change for our staff to work at home.
In March 2020, the work force across the health system was forced to move to remote locations due to the COVID-19 pandemic and the need for safe social distancing. We discovered that care managers could review the electronic medical record and assess and coordinate care by telephone remotely. This experience demonstrated we could move some of our CMs to work remotely, while a portion remained in the hospital. The remainder of our UM staff, as well as our entire Care Management Resource Center, moved to home-based work. We were able to do this with confidence because many of the UM caregivers, as well as the UM Resource Center staff have been working from home part time, with excellent results and data to support the work at home program. An expansion of that program was much easier to accomplish and justify to nursing leadership.
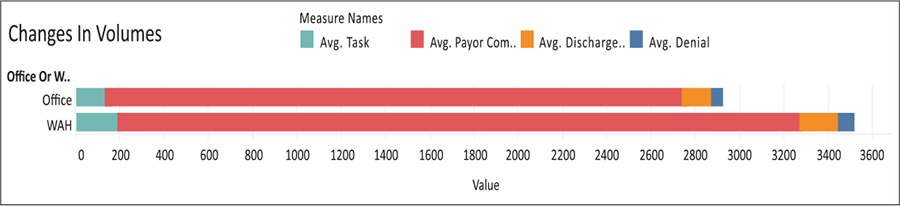
The first important factor to consider when determining the efficacy of a Work At Home (WAH) program would be the staff’s measured productivity. Above are metrics for the Utilization Management Resource Center staff who are in the WAH program, compared to the same staff when they worked in the office (Fig. 1). As you can see, we have seen an increase of nearly 17% of tasks completed per user per month since moving to remote positions.
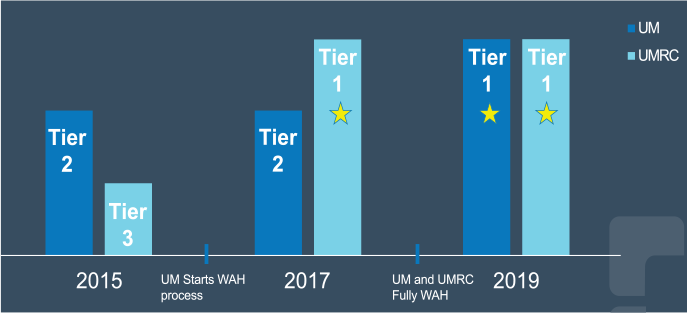
Similar results were found in the utilization management nursing positions (Fig. 2). The graph represents the percentage increase in each year since being home. With the exception of 2019, which included a pilot program in a significant number of our hospitals that eliminated data from our records, we have been averaging an increase of 15.2% in the number of reviews the UM staff have performed each day since going home.

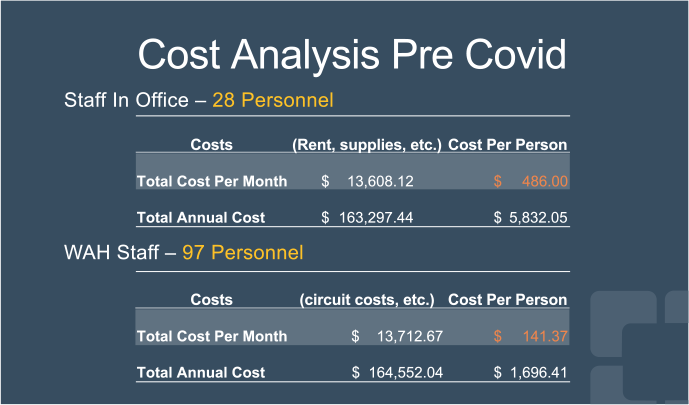
A second important reason for this change was the cost savings to the organization. The current cost of space for rent, supplies, etc. is $13,608.12 per month for the caregivers who remained in the office – the final 25% of the UM team and the entirety of the Resource Center, (in total, 28 staff). The cost per person is $486.00 per month.
The current WAH Program cost is $13,712.67 per month for 97 caregivers. The cost per caregiver working at home is $141.37 per month. There is a significant financial saving to support the WAH Program caregivers. If the 97 registered nurse caregivers were to come back to an office setting, we would require six times the amount of space based on the COVID restrictions. Additionally, the utilization review productivity metrics have garnered an overall productivity increase of 15.2% since the inception of Work at Home in 2016.
Another integral part of the success of the WAH program within the Cleveland Clinic was the satisfaction of our caregivers. The Cleveland Clinic constantly monitors our staff’s engagement and fulfillment in their positions in a number of ways. Turnover rate, engagement surveys and utilization of Family Medical Leave (FML) or Unscheduled Paid Time Off (UPTO) (Fig. 4) have proven to be useful proxies for understanding how the staff are feeling about the work that they do.
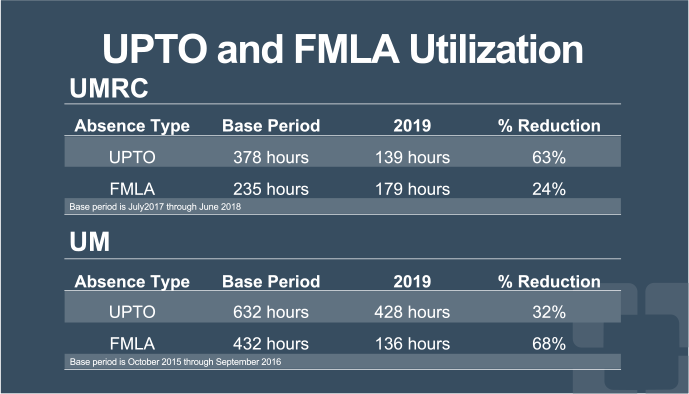
Across the board, when moving to a remote workforce, there were improvements in those areas. For a staff of roughly one hundred, there were four who left the organization in the 2019 calendar year. Only one of those caregivers left for something other than a promotion or job change after achieving a new degree. Similarly, our Press Ganey survey scores improved each survey year since moving the staff home (Fig. 5). There was a bit of a learning curve for our staff and managers to continue to retain the sense of team while not sharing an office space together, but we now see that they are more of a team than ever!
Because of this clear success in sending UM and UM Resource staff home, we were able to quickly replicate the system for the remainder of UM nursing staff and Care Management Resource Center; alleviating financial burden to our health system in a time when every cent counts and providing our staff with safe, effective workflow tools to do their jobs to the top of their licensure. Additionally, because of the success shown by the UM team in working from home, others within the organization were able to replicate similar WAH strategies. Without the clear data showing the positive impacts of the WAH Program, executive leadership would not have been so quick to adopt this strategy. The healthcare world was dramatically altered by the COVID-19 virus in the beginning of 2020; however, the Cleveland Clinic CM Operations department has shown that despite the changes brought on by this pandemic, the future is bright for the support of remote positions across care management in general. Our hope as a health system would be to continue to support the WAH Program for care management staff in selected roles and replicate the successes we have seen so clearly in our data.




