
The Impact of Value-Based Social Care on Health Equity
BY , MBA-HCM, EXECUTIVE DIRECTOR OF CAREADVISORS
As value-based care programs are adopted across the country, it’s no surprise to healthcare providers that all predictions point to an increase in alternative payment models. Social care management that addresses economic stability, housing, food insecurity, employment and other social determinants of health allow value-based care programs to deliver greater value to patients and providers by decreasing the constricted access to social services that impact health inequities.
Three years ago, CareAdvisors had a vision to transform the foundation of social services with automation. My son, Chris, who is the company’s chief executive officer, and I were inspired by an unfortunate experience when a family member passed away without access to desperately needed social service programs. We were determined to use this painful lesson as the catalyst to make a transformative impact on people’s lives.
Today, more than 100 million people struggle to access social service benefits like basic health insurance, as well as emergency cash and food assistance programs. At CareAdvisors, we are expanding the use of advanced automation to replace antiquated infrastructure and provide universal access to social services. We focus our efforts on offering social care automation for the social services that have an effect on healthcare for vulnerable populations including low-income, older adults and persons with disabilities. Our platform automates the enrollment process to increase capacity for a 10X improvement in case management efficiency. We understand how important it is to increase the capacity of your care coordinators and social workers and allow them to focus on the delivery of care and reaching more patients.
Case managers play a critical role in CareAdvisors’ work, and across the healthcare industry. The passion and commitment case managers have to patient education and advocacy makes the difference in positive outcomes. They serve as a vital resource to help people identify and choose resources based on their availability and what best suits the patient’s financial and personal needs. For us, collaborating with case managers and social workers has been a key component to having a positive impact on these vulnerable populations. We rely on the expertise of case managers, evaluating and understanding care options, determining what is best to meet their needs and implementing the tactics needed to bring solutions to patients and their families. This case management process and the partnership with social workers on the front lines has made a difference in addressing social determinants of health (SDoH).
SDoH has been a growing concern for many years, and the COVID-19 pandemic has only exacerbated the problem. For example, in Illinois, one out of every seven people in Cook County will experience food insecurity this year, according to Feeding America’s Map the Meal Gap Study. And while the issue varies greatly, in some communities, up to 50% of residents are food insecure. (Greater Chicago Food Depository, “Hunger Across Cook County” https://www.chicagosfoodbank.org/hunger-in-our-community/). Sadly, many food insecure households do not qualify for the Supplemental Nutrition Assistance Program (SNAP) and have turned to food banks and pantries, soup kitchens and mobile programs for the first time, creating a greater burden on an already stressed system.
A September 2020 CareAdvisors survey of Chicago-area social workers revealed that food insecurity rose from 47% to 66% for their patients during the first six months of the pandemic, and economic instability rose significantly, from 46% to 77%. The social workers also noted that their patients saw a rise in housing insecurity.
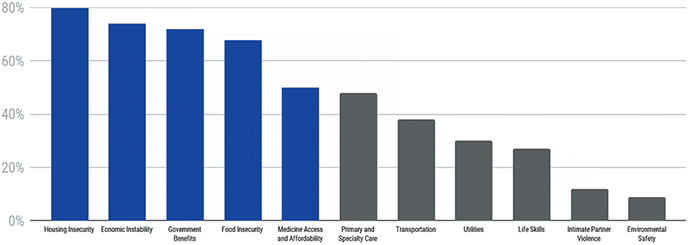
LEADING SOCIAL NEEDS FOR CHICAGO’S VULNERABLE POPULATIONS DURING COVID-19
As patients struggle financially, their access to, and affordability for, healthcare services is constricted. These vulnerable populations can become high-risk patients with complex healthcare and socioeconomic needs, contributing to the cost crisis in healthcare. An example of this high-risk individual is the patient with diabetes who can’t get to a physician because of transportation barriers, who is also suffering with food insecurity and is struggling to access affordable medications.
Progressive hospital and health system leaders know that a key to achieving better outcomes at lower costs is addressing social determinants of health for such patients. Flagging these patients before discharge and putting programs in place to treat patients holistically has proven to improve health outcomes and provide equity in preventive care that results in declining emergency department visits and a reduction in readmissions, a notable cost savings.
Successful value-based social care can realize benefits beyond lower medical costs and higher levels of quality care. Increased provider and patient satisfaction are not far behind when leadership encourages an organizational culture committed to standardizing patient-centered, value-based care processes. Care management teams and community navigators play important roles in enhancing these services. (Health Care Payment Learning & Action Network “Roadmap for Driving High Performance in Alternative Payment Models” ©2019 The MITRE Corporation. https://hcp-lan.org/apm-roadmap/).
What would a value-based care team that addressed social services for the high-risk diabetic patient look like? An effective approach begins with collaboration with a community-based organization that can assist with food delivery and transportation services and also includes a registered dietitian, registered nurse health manager, community health assistant, health coach, medication therapy management pharmacist and pantry manager/wellness associate. The care plan is individualized to the patient’s needs. Biometric measures (weight, blood pressure, HbA1c, etc.) and medication usage are tracked regularly. The team should also address care gaps for the patient (mammograms, flu shots, diabetic foot exams, etc.).
This high-quality program structure helps to ensure that patients are receiving a full continuum of care for all health measures. It is a commitment to excellence and a promise to holistic care that defines successful value-based social care.




