Physician Advisor and Care Management Partnership for Effectively Managing Concurrent Denials
Physician advisor leadership, in conjunction with case management expertise, can be an effective tool in discharge planning to manage length of stay in an acute care setting. As a physician advisor, I have worked closely with case management leadership for several years to tackle barriers contributing to extended length of stay. Pre-COVID, I recall rounding on the units with case management managers and touching base with individual case managers to address any barriers they were facing in facilitating discharges. The case managers often felt supported, and, more importantly, they felt seen by leadership to provide the assistance needed in real time to facilitate discharges. I recall carrying a Post-it with names of patients in denied status that I wanted to discuss with case managers. However, over the years, with an increase in the responsibilities of physician advisors and staffing challenges faced by the case management team, we had to think of more efficient and enhanced ways of collaborating. During the COVID-19 pandemic, we were able to create electronic processes for communication and collaboration between the physician advisor and the case management team.
MEDICARE ADVANTAGE AND DENIAL TRENDS
In September 2018, the Department of Health and Humans Services Office of Inspector General (OIG) published a report expressing concerns of inappropriate denials by Medicare Advantage plans (2018). The OIG report reviewed three years’ worth of claims and noted a greater than 75% overturn rate upon appeal (2018). Most recently, in April 2022, the OIG further published concerns about Medicare Advantage plans denying beneficiary access to medically necessary care by issuing inappropriate prior authorization denials (2022). Thus, the OIG recommended that the Centers for Medicare & Medicaid Services (CMS) increase its oversight of Medicare Advantage plans. However, despite the OIG’s concerns, Medicare Advantage plans continue to grow rapidly, as Medicare Advantage enrollment has more than doubled over the past decade. According to the Kaiser Permanente Foundation report, Medicare Advantage is expected to hold almost 62% of the Medicare share by 2030 (2022). More importantly, according to a study by Change Healthcare, a review of 100 million claims over the past decade indicated an increase in denial rate of more than 20% (2020). These reports and studies highlight that healthcare systems need to effectively utilize all resources available to tackle denials and ensure that appropriate payments are secured for services provided to beneficiaries.
Physician advisors are uniquely positioned to have in-depth understanding of payer contract terms, appeal options, discharge planning as well as clinical rationale for acute hospitalization. Similar to the integral role of the physician advisor in the care management process, the case management team is the appropriate expert in identifying discharge barriers, leveraging Medicare notices and formulating a safe discharge plan. Consequently, collaboration between physician advisors and the case management team is paramount in ensuring timely discharge of patients, especially those with concurrent denials.
CONCURRENT DENIALS: FOUR CATEGORIES OF PATIENTS
Concurrent denials refer to denial of level of care while the patient is still in the facility. At my institution, the denial team, including physician advisors, meets with case managers at least twice a week to review in-house patients in a “denied” status to help expedite discharge. During this meeting, we work together to identify and resolve barriers as well as select appropriate strategies including various relevant denial categories. We categorize concurrent denials into different buckets based on presence of medical necessity and discharge plan availability. It is worth noting that patients can easily go from one category to another during their hospital stay.
Figure 1: Concurrent Denial Patient Categories
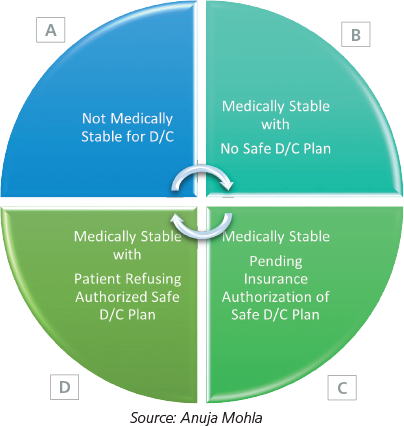
Category A refers to concurrent denial patients who have continued medical necessity. It is important for physician advisors to leverage the payer dispute process by performing a reconsideration and/or a peer-to-peer review within the contracted time frame. However, if the payer upholds the denial, the physician advisor and case management team can work together to place early referrals for post-acute services and discuss an alternate medical plan when feasible. These interventions can make a significant impact on length of stay. For example, physician advisors can help with early identification of patients appropriate for long-term acute care hospitals while the case management team can utilize their vast knowledge about various rehabilitation facilities to identify patients for single case agreements.
Category B refers to concurrent denial patients who are medically stable for discharge without a safe discharge plan. This category requires great oversight from the case management and utilization management team. Besides placing choice-based referrals for relevant post-acute services, it may require physician advisor and case management oversight to expand referrals to additional in-state and out-of-state facilities. For instance, patients taking expensive outpatient medications, patients at risk of psychiatric decompensation or patients with isolation requirements are likely appropriate for upfront broad referrals to facilitate a timely discharge.
Category C includes patients in concurrent denial who are medically stable for discharge with a clear safe discharge plan but pending authorization of post-acute services by the payer. It is important for case managers to have a clear line of communication with the utilization management team and physician advisors to help escalate payer delays for real-time resolution. It is not uncommon for acute hospitals to receive a concurrent denial on a patient who is also pending authorization for discharge to an acute rehabilitation facility by the payer. These situations can be promptly resolved by a physician advisor’s intervention in leveraging their payer contacts, including having a direct line of communication with payer medical directors to help expedite authorization of post-acute services.
Category D includes patients with a concurrent denial with an authorized discharge plan from the payer, but the patient refuses the safe discharge plan outlined by the case manager. This category seems to be the most challenging for case managers as they have worked hard to delineate a safe discharge plan, but the patient may refuse the suggested approach for various reasons. This could include patients being transferred back to the referring acute hospital or to a post-acute facility. Again, these patients may represent the low-hanging fruit where physician advisor and case management leadership can effectively work together on brainstorming potential solutions. Depending on payer and regulatory guidelines, a notice of non-coverage can be issued to the patient to help motivate compliance with the delineated safe discharge plan. Physician advisors and case management together can brainstorm alternate discharge plans, communicate with patients, involve the legal team and escalate to senior leadership as needed to facilitate a timely discharge.
The physician advisor and case manager have different skill sets and expertise that complement one another and allow for significant impact on the length of stay of the patient. This partnership between the physician advisor and case management is critical to the effective management of length of stay for patients in a “denied” status and, ultimately, the effective utilization of resources for healthcare systems.
REFERENCES
The Change Healthcare 2020 Revenue Cycle Denials Index. Change Healthcare. (2020). Retrieved from https://www.changehealthcare.com/insights/denials-index.
Medicare Advantage in 2022: Enrollment Update and Key Trends. Kaiser Permanente Foundation. (Sept 2022). Retrieved from Medicare Advantage in 2022: Enrollment Update and Key Trends | KFF (https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2022-enrollment-update-and-key-trends/).
Medicare Advantage Appeal Outcomes and Audit Findings Raise Concerns About Service and Payment Denials. U.S. Department of Health and Human Service. Office of Inspector General. (2018, September). OEI-09-16-00410 Retrieved from https://oig.hhs.gov/oei/reports/oei-09-16-00410.pdf.
Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care. U.S. Department of Health and Human Service. Office of Inspector General. (2022, April). OEI-09-18-00260 Retrieved from https://oig.hhs.gov/oei/reports/oei-09-18-00260.pdf.





