Receiving timely, accurate and complete information supports case managers in their duty to patients for coordinating care, supporting return to activity and advocating for improved health. Research has shown that communication is a key barrier in slowing down claim processing (reference 1). One common challenge is getting a response from physician offices, which are often busy and focused exclusively on treatment. Case or claim managers providing support post-treatment may require clinician input such as recommended limitations to activities that may hinder recovery, updates to treatment plans or additional documentation to process work leave paperwork.
With many physician offices still using older technologies, like fax machines, the question persists: How can we improve care delivery with more efficient communications?
SURVEYING CASE MANAGERS
To investigate improving these interactions, our research team created an online, anonymous survey that was emailed to case managers involved in U.S.-based, non workers’ compensation, short-term disability claims management or supervisors of claims managers. There were 217 survey responses describing successes and barriers of case managers interacting with physician offices.
For those who responded, 37% needed clinician input on less than a quarter of their claims, but 28% needed input on nearly all their claims. Most were requesting information about the return-to-work plan, care plan or extending a work leave. Over the previous 6 months, the average number of clinician offices that this group was reaching out to was 24 unique offices, but it ranged from 0 to 50 (the max range included in the survey).
The majority of respondents rated their communications with clinics as “good” or “neutral.” Participants commented that major barriers to getting the information they needed from a doctor’s office included poor procedures, poor documentation, unfamiliarity, unwillingness and overloaded clinics. It is noteworthy that outsourced medical records facilities and data sharing issues were described as major drivers for non-response.
RESEARCH TO PRACTICE
According to the respondents, for cases that went smoothly, actionable ideas that case managers could apply included:
- providing detailed and easy to understand requests for documentation
- utilizing the patient as an advocate to complete paperwork
When analyzing the results, significant positive correlations were found between claim managers with more experience and a higher perceived likelihood that clinicians would positively respond to non-clinical information. Specifically, experienced case managers indicated that if they could easily provide data to the clinicians, the most valued topics would include:
- common reasons why patients fail to recover (r =.150, p<.05)
- the patient’s daily work tasks related to their diagnosis (r =.153, p<.05)
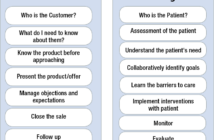
This demonstrates that keeping a two-way communication strategy is likely a key tool for case managers to improve patient outcomes. Even without a clinical background, case managers can do the leg work to gather relevant information that may assist the clinician with decision making, such as sharing the patient’s daily expected activities, population-level recovery estimates or common non-clinical reasons why healing can be delayed.
Further recommendations from the survey included that forms requesting information from a clinician must be straightforward and provide context about relevancy. It was noted in our results that sometimes busy clinician offices do not understand the information being requested or why. Therefore, we recommend developing easy-to-use forms with specific instructions and perhaps a personal note about how this paperwork is supporting the patient.
It may be valuable for organizations to set up procedures for reaching out to clinicians, such as fax number phone banks or recommended checklists including follow-up protocols. When case managers contact physician offices, they should attempt to integrate evidence-based guidelines into their communications to increase efficiencies around each touch point to align better delivery of care. Survey respondents also had success when including the patient in the request for information, so the patient was likewise advocating for the completed paperwork.
These best-practice strategies can help improve communications with physician offices to ensure that case managers at all levels of experience can streamline claim progression.
IMPACT
There are key contact points throughout the life of a claim, and the communication between case manager and the clinician is one of the critical junctures that can help improve efficiencies. Physicians and nurse practitioners have the knowledge and skills to determine when patients can safely return to their normal activities, such as work, and if there need to be limitations, such as an inability to lift or stand for long periods of time until full recovery is achieved. The case manager can enhance that recommendation for the patient by utilizing online evidence-based guidelines to develop a patient-specific, proactive management plan, such as reviewing the patient’s job description and offering advice that perhaps additional breaks or a sit/stand chair would allow the patient to safely return to their job. Then the patient can work with their employer to find tasks that meet the physician’s recommendations. Getting a patient back to their normal routine, or as close as possible, supports both mental health and financial stability for the patient (reference 3).
Communications should also flow in the other direction, with case managers doing the background work to provide helpful information to clinicians so that limitations match the patient’s physical and cognitive abilities with the job requirements and essential functions. The goal is to work as a team with the patient as the focus, but it can be difficult when these “teams” have varying interaction with the claim, the patient or the different members do not understand the importance of one another. Each decision and contact point has a ripple effect within the life of a claim; therefore, these key interactions can collectively influence the patient returning to their job healthily and efficiently.
Leveraging evidence-based resources can be useful for return-to-work cases where there is a need for temporary or permanent workplace integration of an employee with a disability or functional restrictions. Case managers do not need to reinvent the wheel for each patient. There are subscription-based data sources as well as free information that can utilized to bring in data-driven solutions. For example, MDGuidelines provides condition-specific recovery timelines, the Job Accommodation Network offers practical guidance on how to meet Title I of the Americans with Disabilities Act and O∗NET lists occupation-specific data. Resources such as these can be used independently or in conjunction with one another to build an appropriate patient-specific management plan that provides the most realistic return to activity outlook for the patient.
BEST-CASE SCENARIO
Let’s walk through an example of applying some of these strategies: Case Manager Cristina is working with her client, Eric, to extend his short-term work leave from carpal tunnel release surgery.
- Cristina fills out an information request template that utilizes checkboxes and fill-in-the-blank questions to specifically describe what information is needed from the doctor and how it will be used to help Eric continue to receive his employer-based benefits until he can return to the office.
- She includes a short description about his sedentary desk job in the technology industry that requires him to be on a computer typing several hours a day, which Eric is worried will exacerbate his condition.
- Cristina uses the phone bank she has to look up current contact information from the doctor’s office. She also asks Eric to call the office directly to request they complete the form.
- The paperwork comes back in 1 day, indicating that the leave does not need to be extended but there are limitations Eric needs to follow as he returns to activity, including avoiding heavy lifting or doing repetitive arm/hand movements until he reaches 2 weeks post-surgery.
- Cristina reviews an online accommodation guideline and then explains the limitations to Eric so they can discuss alternative work tasks that meet the doctor’s specifications and, in turn, Eric can propose them to his employer. They also brainstorm about accommodations he can ask for to prevent future carpal tunnel issues, including an ergonomic keyboard.
Eric has a successful conversation with his employer, and he plans to go back to the office a few days early to attend trainings that do not involve typing or wrist movement. He will also be getting a sit-stand desk and computer equipment to aid wrist health. Eric feels supported by his employer, can get his full paycheck again and return to work safely.
Ultimately, the information exchange between case managers and physician offices is paramount in efficient delivery of care. Furthermore, improving communication strategies and offering collaborative learning can be protective against case manager burnout (reference 4). High-intensity case management, including small caseloads, regular meetings and close contact with physicians are the most effective strategies to positively impact patient outcomes (reference 2). However, these solutions are less applicable to third-party claims managers because of the high volume of stakeholders, including multiple insurers, health systems and employers. This article offers some tangible steps case or claim managers can take to prevent or overcome communication barriers, even if we are still stuck with fax machines occasionally.
, PhD, is a senior analytics consultant at ReedGroup and has a doctoral degree in industrial-organizational psychology with more than 10 years of experience in data analysis focusing on workplace productivity.


 Keemia Vaghef
Keemia Vaghef Kerri Wizner
Kerri Wizner