Caring for elderly parents and preparing for their end of life is the most difficult time. For baby boomers, it comes at a time when they are preparing for retirement and making plans for a relaxing future. Baby boomers are living longer thanks to better healthcare. Many of their parents are physically declining, and the time of caring for them has come. How does one begin to discuss end of life choices with one’s parent(s) and their healthcare provider? The very words “hospice” or “palliative care” are ones that nobody wants to discuss or think about. It is something we’d like to deal with at a later time. Unfortunately, that time can happen quickly, and a decision will be necessary. End of life choices are difficult, and these decisions affect every person and every family. Case managers can assist with addressing quality and end of life issues as well as honoring the patient’s end of life wishes.
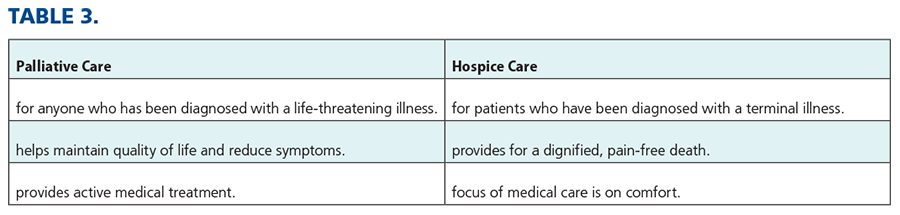
This article will address the difference between hospice and palliative care. It will explain the medical and financial requirements one needs to meet for insurance coverage.
DEFINITIONS
- Palliative care is compassionate comfort care that provides relief from the symptoms and physical and mental stress of a serious or life-limiting illness. Palliative care can be pursued at diagnosis, during curative treatment and follow-up, and at the end of life. Palliative care grew out of the hospice movement.
- Hospice care is compassionate comfort care (as opposed to curative care). Hospice care is for people facing a terminal illness with a prognosis of six months or less, based on their physician’s estimate if the disease runs its course as expected. It is a type of medical care that gives seriously ill patients and their loved one meaningful time together. This is when the focus of care turns from one of active treatment to providing comfort and ensuring there’s quality to their life as the end nears.
PALLIATIVE CARE
- To palliate is “to make a disease or its symptoms less severe or unpleasant without removing the cause.”
Palliative care can begin at the discretion of the physician and patient at any time, at any stage of illness, terminal or not. It usually begins at the time of the medical diagnosis and when treatment is started. While receiving palliative care, patients can continue to see their regular provider or PCP for treatment of their illness or disease. Palliative care remains underutilized and often undervalued.
Patients with cancer, dementia/Alzheimer’s, HIV/AIDS, ALS, COVID-19, and heart, lung, and kidney disease can benefit from palliative care. Palliative care can address common physical problems such as pain, trouble sleeping, shortness of breath, loss of appetite, and nausea. Also included are medication, nutritional guidance, physical therapy, occupational therapy, and integrative therapies. In addition to providing comfort, palliative care can address emotional, social, and spiritual issues. Patients and families often experience high levels of stress and fear, which can lead to anxiety and feelings of hopelessness and depression. Palliative care can provide resources to assist the family and patient through this difficult time.
Palliative care can be offered in hospitals, cancer centers, long-term care facilities, hospice facilities, or at home with care provided by family or agencies. Although there is sometimes limited access to palliative care in rural areas, most hospitals now have palliative care specialists or teams composed of RNs, social workers, and physicians. Other integral members of the team include case managers, CNPs, physicians from different specialties, physician assistants, registered dieticians, psychologists, massage therapists, and chaplains. These team members can offer assistance with counseling, support groups/mental health referrals, and family meetings. They can also help with practical problems such as money/finances, job-related problems, insurance questions, insurance coverage and co-pays, legal issues, and understanding and completing complex medical forms. The palliative care team can coordinate care and provide support for the patient and family while ensuring comfort during the end of life. The ultimate goal is “death with dignity.”
FINANCIAL ISSUES
Coverage for comfort-focused palliative care varies by provider and insurance plan. Each client’s plan may be different. Encourage the patient or family to contact the insurance carrier and inquire about coverage, exclusions, co-pays, out of pocket costs, and coinsurance. Palliative care clients do not have to meet the same Medicare eligibility requirements as hospice patients. Medicare Part B and Medicaid cover some types of palliative care. There may be co-pays for some treatments and medications that are not covered.
Costs of care at the end of life have continued to rise.
COVID-19
With COVID-19, palliative care is as critically needed as fluids, fever reducers, and ventilators. In the case of many COVID-19 patients, there needs to be a rapid assessment of the patient’s goals to align the treatment with the patient’s wishes. This assessment can avoid unwanted procedures. If resources are stretched, some patients may not be prioritized for intensive care and instead may need palliative care. Or the patient may choose not to be admitted to intensive care and opt for palliative care.
If ventilators or intensive care beds are in short supply, hospitals may need to triage patients and communicate with patients and families to develop a treatment plan. That treatment plan could include palliative care. Families may have no visitation or limited visitation. Treatment options may require long-distance communication between the patient, family, and healthcare providers, and this could lead to miscommunication. Written advance directives play an important role in this type of situation as increased attention is now placed on legal documents to guide actions and for decision making. The case manager can assist the family in understanding the situation so that a decision can be made that agrees with the patient’s wishes.
HAVING A CONVERSATION ABOUT THE END OF LIFE
The end of life is a personal experience. It is a unique and subjective experience for everyone. Many people find it difficult to talk about or plan their end-of-life care. Patients may have strong opinions about how they want to be treated and cared for in their final months, weeks, and days. Early discussion(s) may help prevent family disagreements when the end-of-life process begins. Don’t wait for a crisis to occur! Loved ones should be involved early – preferably before palliative care is needed. The discussion should include where they want this care to take place (home, long-term facility, hospital). Research has found that the patient’s main concern is the loss of dignity when dying – and not necessarily the fear of experiencing uncontrolled pain. The majority of patients want their death to be peaceful and dignified with compassion and respect for their wishes or preferences.
- Only 27% of Americans report having talked with their families about their end of life care decisions.
ADVANCE DIRECTIVES
Advance directives are the most reliable way to ensure end of life wishes are honored. Medical decisions/choices should be in writing. Advance directives legally define end-of-life wishes, help avert crises, and ease the decision-making burden for the family, designated caregivers and healthcare team. Advance directives are legal documents composed of two parts: a living will and medical power of attorney. Advance directives need to be signed by a witness and shared with the patient’s family. A great resource is https://prepareforyourcare.org/advance-directives.
Look for the state where the patient resides and download the document.
LIVING WILL
A living will is a legal document that lets a competent adult specify what healthcare the client wants or does not want when the client becomes terminally ill or permanently unconscious and can no longer make their wishes known. It is NOT and does not replace a will, which is used to appoint an executor to manage a person’s estate.
The purpose of a living will is to document the client’s wishes regarding life-sustaining treatment including artificially or technologically supplied nutrition and hydration. A living will doesn’t affect the responsibilities of healthcare personnel to provide comfort care. Comfort care is defined as any measure, medical or nursing procedure, treatment, or intervention, including nutrition and/or hydration, that is taken to diminish a patient’s pain or discomfort but not to postpone death.
If the patient would not choose to limit any or all forms of life-sustaining treatment (including CPR), they have the legal right to do so and should put that in writing.
The patient should consider completing a new living will if their medical condition changes or if they later complete a healthcare power of attorney. Patients should keep copies of their legal papers along with a list of their medications and copies of their insurance information in a secure place at their residence for easy access.
HEALTHCARE POWER OF ATTORNEY
Healthcare power of attorney is a legal document that lets the patient authorize an agent to make healthcare decisions for the patient in most healthcare situations when the patient can no longer make such decisions. Also, the patient can authorize the agent to gather protected health information for and on behalf of the patient. The healthcare power of attorney can make healthcare decisions for the patient whenever the attending physician has determined that the patient has lost the capacity to make informed healthcare decisions. This does not require or imply that a court must declare the patient incompetent. If the patient’s wishes are unclear or unknown for a particular situation, the healthcare power of attorney can make a determination in the patient’s best interests. The healthcare power of attorney is not liable for any breach of duty unless the breach was committed dishonestly, with an improper motive, or with reckless indifference to the purposes of the power of attorney or in the patient’s best interest. The healthcare power of attorney may take any action considered advisable to enforce the patient’s wishes. The healthcare power of attorney has no expiration date. A healthcare power of attorney is not a financial power of attorney an is different from power of attorney.
Each state has guidelines for the healthcare power of attorney (POA). In general, the healthcare POA can:
- consent to the administration of pain-relieving drugs or treatments or procedures (including surgery) that may provide comfort even though such drugs, treatment, or procedures may hasten death.
- make decisions regarding life-sustaining treatment including artificially or technologically supplies nutrition or hydration if there is no living will.
- give, withdraw, or refuse to give informed consent to any healthcare procedure, treatment, interventions, or other measures.
- request, review and receive information (verbal or written) regarding the patient’s physical or mental condition including but not limited to all medical and healthcare needs.
- consent to further disclosure of information and to disclose medical and related information concerning the condition of and treatment to other persons.
- execute any releases or other documents that may be required to obtain medical and related information.
- execute consents, waivers, and releases of liability.
- select, employ, and discharge healthcare personnel and services providing home healthcare.
- select/ contract for admission, transfer, or discharge from any medical or healthcare facility. This includes hospitals, nursing homes, assisted living facilities, hospices, adult homes.
- transport or arrange transportation to a place where the healthcare power of attorney is honored.
- complete and sign for the patient consents to healthcare treatment, issue do not resuscitate (DNR) orders, request to be transferred to another facility, or to be discharged against healthcare advice. In general, the healthcare power of attorney cannot:
- refuse or withdraw informed consent to healthcare necessary to provide comfort care.
- refuse or withdraw consent to healthcare if the patient is pregnant and the refusal or withdrawal of healthcare would terminate the pregnancy unless the pregnancy or the healthcare would pose a substantial risk to the patient’s life or unless the attending physician and at least one other physician to a reasonable degree of medical certainty determine that the fetus would not be born alive.
- order the withdrawal of life-sustaining treatment (including artificially or technologically supplied nutrition or hydration) unless the patient is in a terminal condition or a permanently unconscious state and two physicians have determined that life-sustaining treatment would no longer provide comfort or alleviate pain.
- withdraw treatment that the patient has previously consented to unless the condition has significantly changed and that healthcare is significantly less beneficial or unless the healthcare is not achieving the purpose for which it was chosen.
If a guardian is appointed, the guardian’s duties will include making the day-to-day decisions of a personal nature for the patient including food, clothing, and living arrangements. The healthcare power of attorney remains in effect and controls healthcare decisions unless otherwise determined by the court.
Power of attorney can hold, manage, and control all real and personal property owned by the client and can do all things necessary to protect the client’s interests.
SIDE NOTES
Research has found that patients’ main concern is loss of dignity when dying – and not necessarily the fear of experiencing uncontrolled pain.
Recent findings suggest that cancer patients who receive palliative care alongside standard treatments can live longer.
The majority of patients want their death to be peaceful and dignified, with compassion and respect for their wishes and preferences.
HOSPICE: WHAT IS IT?
- A medical designation given by a physician certifying that a person’s life expectancy is six months or less. Occurs when the patient no longer has medical options or has chosen not to pursue further treatment. Hospice offers symptom relief and comfort from pain. Additionally, it’s a word indicating a place where one spends their final time with family and friends. Here comfort care without curative intent can be provided. Hospice is most often provided in a patient’s current living setting such as their home/apartment, skilled nursing home, or assisted living facility. Some hospice providers can offer services in a hospice facility, or within a designated hospital floor. No matter which location, it’s where meaningful time can be spent in ones’ final days. A full range of services can be offered that puts patients and families in control of medical choices during this difficult time.
THE HOSPICE TEAM
No matter the patient’s chosen location for their hospice designation, they will have a competent team to assist them and their family through this end of life journey. Members of this team can include the following individuals, who are similar to those of the palliative team. Case managers and social workers help coordinate care and address any emotional, financial, or social stresses the patient is faced with. The patient’s personal physicians and/or a hospice physician have expertise in pain and symptom management. A registered nurse can supervise the determined plan of care and provide any hands-on care or training of the determined family caregivers or those assigned through an agency. Hospice aides/caregivers are needed for personal assistance in ADLs. Chaplains can be called upon to provide pastoral care of the patient’s choice.
FINANCIAL REQUIREMENTS/RESPONSIBILITIES
For those patients who are non-eligible Medicare/Medicaid patients, hospice payments may come from private insurance or an HMO. Both include hospice benefits, and they employ financial specialists to assist those who do not qualify for federal programs nor have private insurance. All hospice organizations are reimbursed the same.
Hospice Medicare-eligible patients must have Medicare Part A (hospital insurance) to receive payment coverage. They will need a physician to certify they have a life expectancy of 6 months or less. Also, the patient chooses to receive only comfort care and not medical treatment aimed at curing their illness or disease. They are eligible if transitioning from palliative care to hospice care.
MEDICARE HOSPICE CARE COSTS
If the Medicare hospice guidelines are met, then a Medicare hospice provider must provide five levels of care for the patient. These are:
Level 1: routine home care
Level 2: continuous home care
Level 3: general inpatient care
Level 4: respite care for families, when they are the providers
Level 5: covers inpatient hospice room/board in a skilled nursing facility or hospice facility
Only original Medicare covers hospice care costs in these five level locations for a lifetime maximum of 210 days. (This doesn’t include programs through private insurance companies.)
Hospice is the only Medicare benefit that includes all prescription medications, over-the-counter medications, medical equipment and supplies related to the terminal illness, 24/7 access to care, nursing, social services, chaplain visits, grief support following a death, and other services deemed appropriate by the hospice agency. It also includes, PT, OT, ST (only when necessary for ambulation/communication assistance), and dietary counseling. Lab and other diagnostic tests necessary to achieve optimum palliative care are covered. Inpatient care for pain and other symptoms that cannot be managed at home, are included too.
Hospice care covered by Medicare and most insurances DOES NOT cover 24-hour care by family, friends, privately-paid caregivers or staff at a nursing facility.
A person may stay in a federally funded hospice program for more than 6 months, but only if re-certified as still likely to die within 6 months. In this program they can be evaluated monthly for progression of their disease/illness. If necessary, they may be returned to their prior living location until closer to end of life. Note: This doesn’t remove them from a hospice diagnosis.
Hospice patients may go to an ED for care of an injury or condition NOT related to their hospice diagnosis.
99%+ of hospice patients do not have any out-of-pocket expenses.
If a patient is enrolled in a Medicare Advantage Plan, Medicare will still cover the cost of hospice care.
HOSPICE ADDITIONAL NOTES
Should the patient’s health improve, or if they choose, hospice can be stopped at any time. As long as the client meets eligibility criteria, they can return to hospice care. Those who exceed their life expectancy may receive hospice beyond 6 months. There is no penalty for the extended benefits. They would need a physician to reconfirm their terminal diagnosis and have 6 months or less to live. Medicare will continue to cover benefits for any health problems that are not directly related to the terminal illness.
IMPLICATIONS FOR CASE MANAGERS
- Be an advocate for clients and family/caregivers.
- Provide education regarding care options for patients and family/caregivers.
- Collaborate with all healthcare providers involved with the patient’s care.
- Keep the lines of communication open between the patient, caregivers, and healthcare providers.
- Always be an active listener.
SUMMARY
As case managers are challenged by new healthcare issues, palliative and hospice care will play an important role. We must ensure that discussions and decisions regarding initiating, withholding or withdrawing medically necessary healthcare in advanced illnesses and at the end of life are guided by ethical and cultural considerations. These should be based on the patient’s goal of care, preferences, and beliefs. We must ensure interdisciplinary team support for the patients’ and families’ wishes as directed by all types of advance directives. We must keep ourselves educated in the changes that take place in these advance directives. Case managers need to ensure that patients receive compassion and empathy.
The End of Life is Never Certain. Your Wishes/Decisions Should Be Certain. End of life decisions should not be made at the end of life.
REFERENCES
- National Hospice and Palliative Care Organization “Facts and Figures: Hospice Care in America.”
- CMS (Medicare) Hospice Information guides 2019-2020
- Conn’s Current Therapy 2018 Philadelphia, PA
- Linda J Vorvick, MD Clinical Professor UW Medicine, University of Washington, Seattle WA Dept. of Medicine review updates 1/14/2018
- House SA. Palliative and End of Life Care.




