
Collaboration, Communication, Coordination: Moving to Build Consensus for Change
The starting point to moving forward in building consensus for change is to define what I refer to as the 3 Cs, collaboration, communication & coordination. The 3 Cs are integrated initiatives that, when working together, allow organizations, associations, healthcare professionals, care teams and diverse populations to work toward defining common goals for building consensus.
COLLABORATION
According to Indeed.com, collaboration means working together with one or more people to complete a project or task or develop ideas or processes. In the workplace, collaboration occurs when two or more people work together toward a common goal that benefits the team or company. In the healthcare setting, collaboration is defined as healthcare professionals assuming complementary roles and cooperatively working together, sharing responsibility for problem-solving and making decisions to formulate and carry out plans for improvement in patient care (ncbi.nih.gov). A third context I would bring forward is that collaboration, at its best, is when diverse groups of individuals representing competitive organizations choose to come together to address a common issue faced by all and commit to problem solving for the good of the population and/or the community they serve.
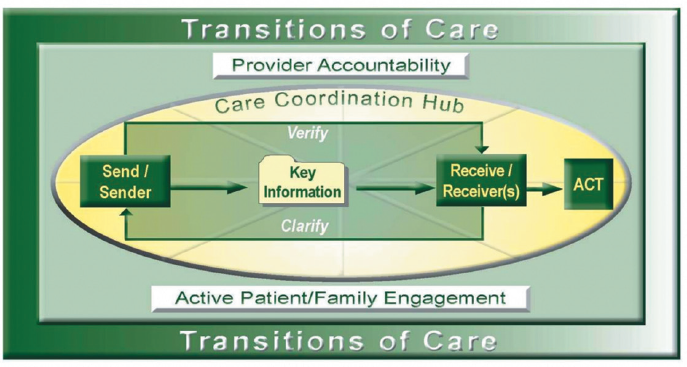
FIGURE 1 SOURCE: National Transition of Care Coalition, Transition of Care Measures, 2008. Used with permission.
COMMUNICATION
Webster’s Dictionary defines communication as “the imparting or interchange of thoughts, opinions, or information by speech, writing or signs.” A definition of communication from Oxford Languages is, “1. the imparting or exchange of information or news, 2. communication means sending and receiving information, such as phone lines or computer.” The National Transitions of Care Coalition (NTOCC) describes the elements of effective communication as the sending and receiving of information, verifying the information is received and if there are any concerns, to clarify those concerns with the sender and obtain relevant answers. Figure 1 shows the key elements of communication related to patient care and transitions (NTOCC, 2008).
It is important to keep the concept of ensuring that the sender and receiver have communicated clearly as we discuss building initiatives where collaboration, communication and coordination become the key building blocks for success.
COORDINATION
According to Management Study Guide, coordination is the unification, integration and synchronization of the efforts of group members so as to provide unity of action in the pursuit of common goals (MSG, 2022). The Agency for Healthcare Research and Quality (AHRQ) states care coordination involves deliberately organizing patient care activities and sharing information among all of the participants concerned with a patient’s care to achieve safer and more effective care (AHRQ, 2022). In other words, when we have committed to collaboration in support of a common goal, using effective communication, clarification and affirmation of the initiative, we then must coordinate the group’s collaborative work and outcomes with unity of action.
The long-term success of coalitions, collaboratives and alliances depends on implementing and using the 3 Cs efficiently and effectively. When we bring various stakeholders together to collaborate on a common purpose, the need to build trust and respect with open and truthful communication is one of the first building blocks that will support the success of that collaboration. Without that, the collaboration effort will be short-lived. Consider also that if we build a strong collaborative and the group is encouraged and feels safe to share their ideas and concerns and there is agreement to implement specific changes, the next step is coordination and dissemination of those changes. If we fail to have the commitment of the various stakeholders to disseminate the information or program, we have supported a wonderful concept only to have it die on the vine. I want to reiterate that just as it takes three legs on a three-legged stool for stability, it takes the 3 Cs supporting each other to be successful in changing systems, processes and outcomes. Transformational change will not happen without the 3 Cs.
In 2006, the National Transitions of Care Coalition (NTOCC) began its journey by convening a group of diverse business leaders and stakeholders from various levels of care services. This initiative was started by the Case Management Society of America and Sanofi-Aventis, now referred to as Sanofi. The common purpose of the first coalition meeting was identifying the issues associated with transitions of care and coming together to discuss how to improve the quality of transitions. To this day, it remains the same. NTOCC convened the stakeholders, providing them with the preliminary objectives to discuss the gaps and barriers with transitions of care and to discuss how we might work together to address the concerns, provide resources and support a safer and improved patient journey at the point of transition. The coalition committed to open and respectful communication during discussions and that accepted recommendations for resources, consensus statements or policy initiatives would be by consensus agreement of the Advisory Council members. The first meetings of the coalition established that the resources and educational library would be available to the healthcare industry at no cost. NTOCC, by consensus vote, did not copyright or trademark its resources so healthcare professionals could use the content to meet the needs of the populations they served. The members of the council, the NTOCC community and those who access today’s resources are encouraged to coordinate and disseminate the information within their organizations and the industry. NTOCC’s success through these 16 years has been staying focused on its mission and using the 3 Cs, collaboration, communication and coordination, to meet the changing needs of the healthcare industry.
Coalitions may be loose associations in which members work for a brief time to achieve a specific goal and disband. They may also become organizations in themselves, with governing bodies, particular community responsibilities, funding and permanence. They may draw from a community, a region, a state or nationally. Regardless of their size and structure, they exist to create and/or support efforts to reach a particular set of goals (Community Tool Box, 2022).
Several lessons have been learned during the 16 years of working with the NTOCC. It was and is imperative that the common purpose, ground rules for engagement and the expected outcomes were set from the very beginning. No surprises for the members, the coalition was convened to reach a specific set of goals for improving transitions of care. Inviting leaders and stakeholders who were shakers and doers was key. Coalitions fail when individuals come to meet but will not work together and then you will have a disruptive environment. Everyone is needed to be open to sharing their experiences and helping members of the council to understanding the concern(s) from their perspective. The coalition was not about complaining or sharing negative attitudes but looking at innovation and collaboration to change the negative outcomes resulting from poor transitions. As a leader working with the coalition and supporting the growth of collaboration, I learned to be ready to listen, to be open and to learn from others, to be flexible and to be willing to adapt when a situation seen as an opportunity presented itself. Listed below are some helpful considerations that leaders convening and building collaboration models or even staff meetings may want to consider.
SUPPORTING MEANINGFUL COLLABORATION
- Ensuring a safe environment for everyone to communicate – members will shut down and not offer suggestions or recommendations if they believe they are not heard or acknowledged.
- Miscommunication or misunderstanding due to the failure to clarify statements. Do not rush communication and do not assume; rather, always confirm.
- Keep an open communication dialogue allowing for creativity with participants and avoid directives.
- Keep the members focused by confirming the mission and vision of the meeting.
- Do not let an individual ramble or take over the discussion.
- Be realistic and stay on agendas and timelines.
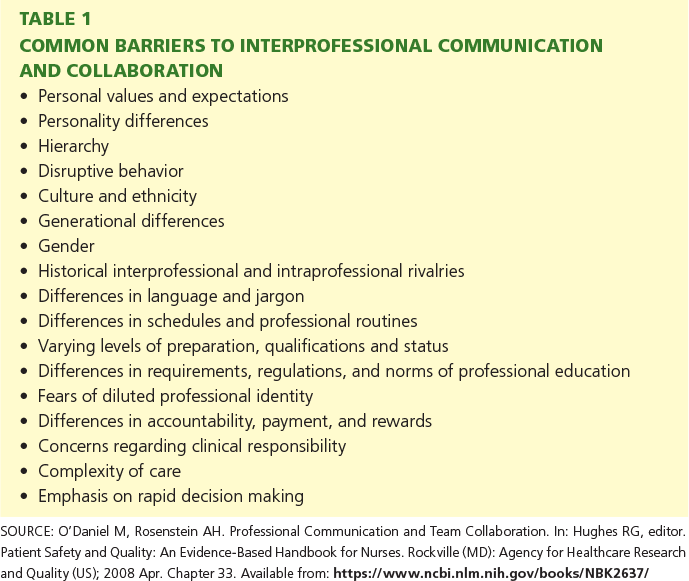
In Patient Safety and Quality: An Evidence-Based Handbook for Nurses, authors Michele O’Daniel and Alan H. Rosenstein in Chapter 33 on Professional Communication and Team Collaboration provided an excellent list of common barriers to effective communication (Table 1). Keeping these in perspective can help avoid negative interactions.
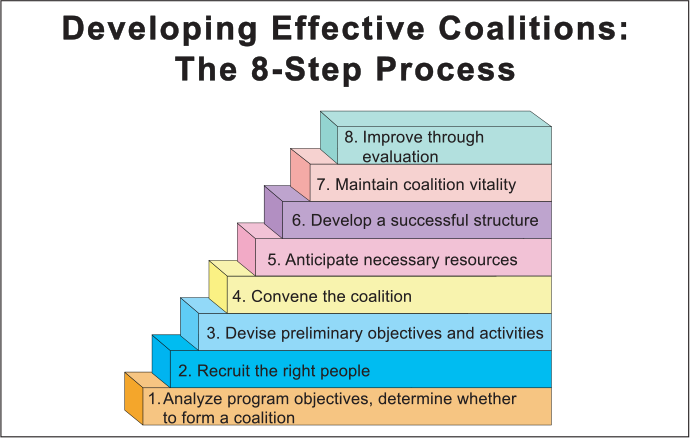
Using Collaboration, Communication and Coordination, no matter whether you are building a coalition, developing interdisciplinary care teams or leading a board meeting is an exciting and rewarding initiative. Those who participate in this process often say, “I feel I may get more from the meeting than I contribute.” I personally learn something new and helpful from each of the coalitions, boards, advisory councils and alliances I have worked with over the last 25 years. A helpful tool when considering developing an effective coalition and using the 3 Cs, is the 8 Step Process from the Preventive Institute (https://www.preventioninstitute.org/publications/developing-effective-coalitions-an-eight-step-guide).
The 3 Cs are needed for many aspects of healthcare today, and the lessons learned here can be applied to staff meetings, medical rounds, case management, board meetings, associations and public policy collaboratives, to mention a few. Much can be learned from collaboration efforts, but the possibilities that are offered when collaboration is a team effort instead of individuals are so much greater. Healthcare professionals must be leaders in this vision of collaborating, communicating and coordinating not only for improving patient care but for ensuring transformational changes in a healthcare system that needs for us to be resilient and open to better ways of working together and delivering quality healthcare.
REFERENCES
Collaborations Skills Definitions and Examples – https://www.indeed.com/career-advice/career-development/collaboration-skills.
O’Daniel, M, Rosenstein, A, Chapter 33 Professional Communication and Team Collaboration – Patient Safety and Quality: An Effective-Based Handbook for Nurses, April 2008, Accessed 6.2022 https://www.ncbi.nlm.nih.gov/books/NBK2637/#:∼:text=Collaboration%20in%20health%20care%20is,out%20plans%20for%20patient%20care.
Oxford Languages Dictionary https://languages.oup.com/research/oxford-english-dictionary/Accessed 6.2022.
Transitions of Care Measures, Paper by the NTOCC Measures Work Group, 2008, Accessed 7.2022 https://static1.squarespace.com/static/5d48b6eb75823b00016db708/t/5d49bc5dc8a2700001c6ac7e/1565113438113/TOC+Measures.pdf.
The Management Study Guide, accessed 7.2022, https://www.managementstudyguide.com/coordination.htm.
Care Coordination – Care Coordination Atlas, June 2014 https://www.ahrq.gov/ncepcr/care/coordination/atlas.html.
Community Tool Box, Section 5. Coalition Building I: Starting a Coalition, Accessed 7.2022 https://ctb.ku.edu/en/creating-and-maintaining-coalitions-and-partnerships.
Preventive Institute, Developing Effective Coalitions: The 8-Step Process, Accessed 7.2022, https://www.preventioninstitute.org/publications/developing-effective-coalitions-an-eight-step-guide.
Jose Angel Gurria Quotes. (n.d.). BrainyQuote.com. Retrieved July 9, 2022, from BrainyQuote.com Web site: https://www.brainyquote.com/quotes/jose_angel_gurria_890399.





