BY MELANIE A. PRINCE, MSN, BSN, NE-BC, CCM, FAAN
Have you ever used design thinking? I recently did an academic project about this concept. Design thinking is a human-centered approach for complex problem solving, creativity and innovation using dialogue, interactive engagement and learning to address individual biases and challenges to the status quo (Liedtka, J. 2018). Figure 1 is a visual representation of the process as depicted by Real Concepts for Design Thinking.
Figure 1
Design Thinking Loop
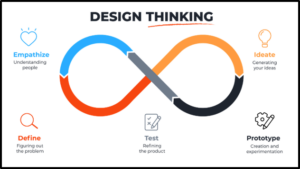
Source: https://www.maqe.com/insight/the-design-thinking-process-how-does-it-work/
The project assignment was to use design thinking to reframe the concept of universal healthcare in the United States and produce innovative solutions to any problems discovered from the process. This article is not about design thinking, but rather behaviors observed in some of the individuals during the brainstorming aspects of design thinking. Specifically, the concept of empathy took center stage as participants problem-solved the health disparity loop. The Stanford University model (Figure 2) has a detailed representation of the design thinking steps and sets the stage for this article’s thesis. Is there an intersection between empathy and health disparity?
Figure 2
Stanford University Design Thinking Flow, (Terrar, D. 2020).
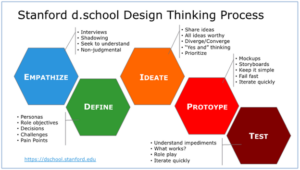
Source: https://dschool.stanford.edu
Health Equity and Disparity
The United States Department of Health and Human Services Healthy People 2010, Healthy People 2020 and Healthy People 2030 have consistently established a goal to eliminate health disparities and achieve health equity for all populations. (DHHS online source, retrieved July 2022). The terms are sometimes used interchangeably, but Braveman, et.al. (2014) does an excellent job of discerning the differences in an article on health disparities and health equity:
“Health equity means social justice in health (i.e., no one is denied the possibility to be healthy for belonging to a group that has historically been economically/socially disadvantaged). Health disparities are the metric we use to measure progress toward achieving health equity” (Braveman, et.al. 2014, p.4).
Healthy People 2030 defines health disparity as:
“a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; gender; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion” (DHHS website, retrieved August 2022).
Lavizzo-Mourey, et.al. (2021) advocated for the need to understand the drivers of health disparities by studying the systematic barriers to unequal access to care. As the authors sought to define disparity, they analyzed a 2003 congressional report titled Unequal Treatment. They found transitions of care between hospital-based, rehabilitation, long-term, home-based and outpatient care contained racial and ethnic disparities associated with unfavorable health outcomes (Lavizzo-Mourey, et.al. 2021).
These definitions of health disparity prompted a somewhat contentious debate by some of the Design Thinking project participants because concepts such as race, ethnicity, religion, gender identity and socioeconomic invoked political perspectives. As depicted in Figure 2, the first phase of Design Thinking is empathy. As the project coach guided the team from the initial discussion on health disparity to the empathy phase of design thinking, perspectives changed. By the end of the project, some of the most provocative perspectives about health disparity literally transformed. This transformation occurred during the empathy phase as participants “walked in the shoes” of others outside of their individual characteristics. But what is empathy, and does it have a bearing on health disparity?
Ratka (2018) observed that empathic people can identify and understand situations, feelings, motives, diverse perspectives and appreciate the concerns of other people. People who are empathetic have the ability to try another person’s life, (Ratka 2018)…what I call “walking in other people’s shoes.” Empathy is expected within our healthcare system and is a foundational principle in many organizations. For example: The Association of American Medical Colleges, the American Association of Colleges of Nursing and accreditation standards for social workers and pharmacists include empathy as an essential learning objective (Ratka, 2018). The Case Management Society of America (2022) incorporates empathy in the standard for client assessment.
Empathy is an observational, affective skill. Mercer, et.al. (2016) conducted an observational study of general practitioners in Scotland analyzing the relationship between empathy and health outcomes. Some of the findings were:
- a lower perception of physician empathy from the deprived groups compared to the affluent groups in the study
- empathy was a predictor of better patient outcomes
- when physicians interacted with the deprived groups, verbal and nonverbal behaviors were less patient-centered than with the affluent groups
- at one month, health outcomes were worse in the deprived versus affluent groups
- patients’ positive perceptions of physician empathy predicted better outcomes in both groups
Ratka’s (2018) studies on empathy as an affective skill supports the Mercer research where empathy was found to have a positive impact on the ability to recognize disparities in healthcare.
The ability to recognize disparities in healthcare will require care professionals to demonstrate skills in empathy and break down “bias barriers” to undertake the challenges of health equity. Lavizzo-Mourey, et.al. (2021) suggested a deeper understanding of structural racism impact on health by addressing the systemic effects of ethnocentrism, homophobia and unequal treatments based on immigration status and sexism on health outcomes. To effectively engage in this complex work, care professionals must first understand the people who are affected by unequal access to care, and it starts with empathy.
Empathy provides the lens through which one can comprehend the social context of patients/clients’ lived experiences as they navigate the healthcare delivery system. The patients/clients cannot be extricated from the society in which they live or the impacts of said society on health and well-being. For decades, health disparity has been studied, documented and taught in forums around the world. The plethora of literature affirms the content for discussion, but the affective skills of empathy provide the context for actionable, innovative ways to pursue the elimination of health disparities.
References
Braveman P. (2014). What are health disparities and health equity? We need to be clear. Public health reports (Washington, D.C. : 1974), 129 Suppl 2(Suppl 2), 5–8. https://doi.org/10.1177/00333549141291S203.
Case Management Society of America. (2022). Standards of practice.
Mercer, S. W., Higgins, M., Bikker, A. M., Fitzpatrick, B., McConnachie, A., Lloyd, S. M., Little, P., & Watt, G. C. (2016). General Practitioners’ Empathy and Health Outcomes: A Prospective Observational Study of Consultations in Areas of High and Low Deprivation. Annals of family medicine, 14(2), 117–124. https://doi.org/10.1370/afm.1910.
Healthy People 2030. Health equity in healthy people 2030. DHHS website. Retrieved July 2022. https://health.gov/healthypeople/priority-areas/health-equity-healthy-people-2030.
Liedtka, J. (2018). Why design thinking works. Harvard Business Review. https://hbr.org/2018/09/why-design-thinking-works.
Lavizzo-Mourey, R., Besser, R. & Williams, D. (2021). Understanding and mitigating health inequities — Past, current, and future directions. New England Journal of Medicine 384:1681-1684. https://doi.org/10.1056/NEJMp2008628.
Ratka A. (2018). Empathy and the development of affective skills. American journal of pharmaceutical education, 82(10), 7192. https://doi.org/10.5688/ajpe7192.
The design thinking process-how does it work. (2020). Retrieved August, 1, 2022. Online source. https://www.maqe.com/insight/the-design-thinking-process-how-does-it-work/.
Terrar, D. (2020). What is design thinking. Retrieved August, 1, 2022. Online source. http://www.theagileelephant.com/what-is-design-thinking/.

Melanie A. Prince, MSN, BSN, NE-BC, CCM, FAAN, is the immediate past president of the Case Management Society of America.
Image credit: ISTOCK.COM/ROMAN DIDKIVSKYI




