BY , MSW
The global COVID-19 pandemic will have significant impacts for both health systems and patients. It is clear there will be economic, clinical, and psychosocial consequences, among others. While these consequences continue to be better understood, especially the magnitude of the financial losses to hospitals, the silver lining during this pandemic is that new, creative, and innovative ways to connect and support patients are now occurring. It is remarkable to witness how these innovative ideas have been implemented in a short amount of time. Although there will continue to be more traditional elements of care, the COVID-19 pandemic is demonstrating how new models in healthcare, such as virtual patient care and digital outreach, can be more readily available to patients. However, case managers and social workers must continue their central role in coordinating patient care just as before the COVID-19 crisis.
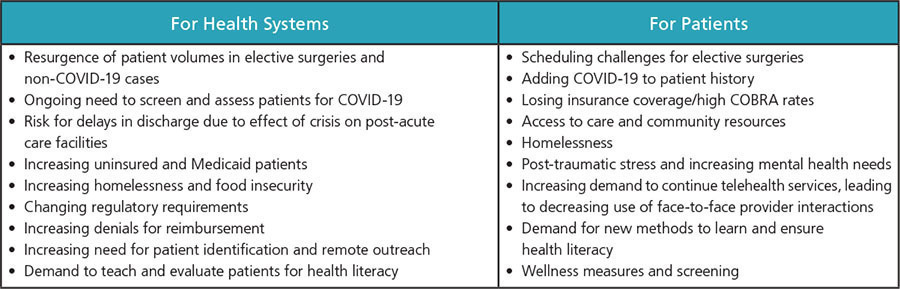
As health systems come back on line during and after the COVID-19 pandemic, the elements in the chart below should be considered for both patients and the systems themselves.
A first step is to consider the current roles of case managers and social workers. These teams are positioned to manage priorities before, during, and after times of crisis. They bring strength and calm to hospital teams, patients, and caregivers. Ensuring an effective and comprehensive case management and social work team will be mission critical to address rebounding volumes, volumes of uninsured/Medicaid patients, increases in discharge delays or lengths of hospital stays, maintaining regulatory compliance, patient identification and outreach, denial and pre-authorization management, emotional wellness, and an enhanced need for effective communication.
REBOUNDING VOLUMES
Case managers must work closely with bed management and patient insurance verification to ensure timely authorizations and bed availability. Case managers in the hospital and at the entry points will be essential components of the care initiative. Additionally, post-acute care facilities will become less available due to higher volumes of COVID-19 patient influx and must be addressed. The increased demand on home-based care must also be evaluated, along with greater collaboration with home care agencies.
ESCALATING VOLUMES IN UNINSURED AND MEDICAID
The increasing number of patients needing assistance through federal government programs such as Medicaid, food assistance programs, disability and other social safety net programs will require more resources from social workers and case managers. This will not only impact patients who have lost their medical insurance, but there may also be an increase in homelessness. Research indicates that patients without insurance and/or who are homeless have longer lengths of stay in the hospital, higher incidence of readmissions, and high volumes of unnecessary emergency department visits. Case management and social work can play a role here as well, through interventions with patients dealing with homelessness.
INCREASING DISCHARGE DELAYS AND LENGTH OF STAY
There has been a tremendous strain put on the post-acute care network, which will likely continue. The COVID-19 crisis has created escalating scrutiny on the decision to accept patients with COVID-19 or post-COVID-19 patients from the hospital. Case managers and social workers must ensure early identification of the need for post-acute care and community connections proactively. It will be important to avoid “bed wars” between case managers vying for the same bed. New strategies and collaboratives in discharge planning will be imperative.
REGULATORY COMPLIANCE
As CMS brings regulatory requirements back online, it will be critical for hospitals to be aware of any regulatory changes and when regulatory compliance practices have resumed. It is possible that some of the regulatory requirements (such as 3-day IP stay) could be eliminated.
PATIENT IDENTIFICATION & OUTREACH
Case management and social work evaluations will need to include a patient’s COVID-19 history (including exposures and the aftercare received). Bolstering high-risk identification processes and hand-offs to ambulatory services will allow case managers to help patients avoid long-term follow up and readmission. Identifying and conducting outreach to patients in the immediate future is needed, preferably before a second wave of COVID-19 occurs.
DENIALS MANAGEMENT AND PRE-AUTHORIZATIONS
As elective surgeries return and hospitals need swift authorizations for surgery and post-acute care, case managers are essential. Having case management support in place will help manage and mitigate the impact of denials and excessive back-end processes on patients and providers.
EMOTIONAL WELLNESS AND MENTAL HEALTH NEEDS
Patients and their families will have potentially long-lasting psychological or psychosocial effects from the COVID-19 pandemic, especially if a person was infected or was isolated. As a consequence of these effects, it is likely that patients will witness social admissions, unnecessary ED visits, or delayed discharges. It is essential to arm your social work team with the tools and techniques to provide patient support and know the referral resources in the area. Additionally, overwhelmed systems facing ongoing and delayed chronic care patients, with the right case managers and social workers in place, will now feel more confident.
This will not just affect the patients, but it will also affect the team caring for these patients. Social workers are uniquely positioned to support the teams through collaborative interventions, critical incident debriefing, and other tactics in supporting individuals and teams through crisis.
EDUCATION/TEACHING TOOLS
Case managers are highly sympathetic and insightful patient advocates and educators. They can prepare patients and families to address and anticipate different ways to manage their medical needs and information. Because health systems and providers are gaining a better understanding of COVID-19 and the processes, programs, providers, and tools that are essential, having experienced case managers and social workers in place to help educate and teach families about their medical needs is necessary.
ENHANCED EXPECTATIONS FOR COMMUNICATION
There is a significant gap in communications between healthcare providers and family members. Understaffing and unclear expectations on the part of front-line personnel for when and how information is communicated to family members and other stakeholders must be addressed. Case managers and social workers are excellent front-line communicators in these scenarios.
Organizations need to continue using technology as a means of effective and efficient clinical service communication to patients. Over time, patients will become more accustomed to this form of communication. Telehealth, payer telephonic liaisons, community advocates, kiosks, and avatars are many of the existing tools of communication. Case managers and their social work partners have the patience and knowledge to communicate and assess the strengths of these tools to support families during this time.
Case managers and social workers have always supported patients and their families in times of crisis. They will take on the challenges of COVID-19 as well; as contemporary team members, partners, and patient advocates.





