
Telehealth: A Healthcare Certainty In Uncertain Times
BY
Certainty is, to say the least, a limited commodity these days. But a genuine consensus across healthcare has emerged that telehealth, done right, can be an important tool for providing care more effectively to more people. And tracking the quality of the care provided via telehealth is imperative.
The National Committee for Quality Assurance (NCQA) is already incorporating telehealth into our quality measures and programs. We convened thought leaders across the health sector and in government to form the Taskforce on Telehealth Policy (TTP) to build consensus for moving forward.
Despite much greater use and appreciation of telehealth, we do not have broad consensus on standards for its safe, effective, and appropriate use in promoting high-quality care, and there are lingering concerns about potential inappropriate use, patient harm, fraud, waste and abuse.
A health system that fully incorporates optimal use of telehealth with clear standards for its safe, effective, and appropriate use in promoting high quality, well-coordinated care.
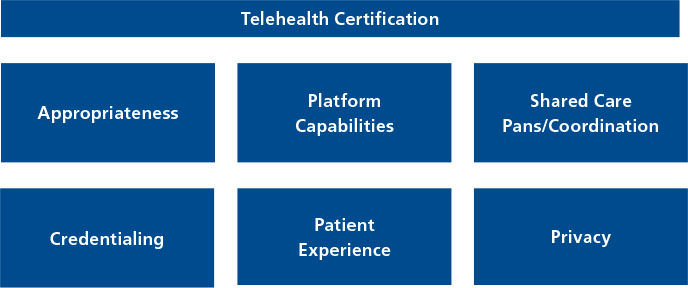
There is growing consensus that we need clear criteria for certifying safe, effective, appropriate and patient-centered telehealth use, as seen in the TTP’s consensus recommendations. Standards for this can include:
- criteria for when telehealth is and is not appropriate to ensure patient safety,
- clearly defined platform capabilities,
- shared care plans and active care coordination among all members of patients’ care teams – not just telehealth,
- measuring patient telehealthcare experience,
- provider credentialing, and
- privacy protections.
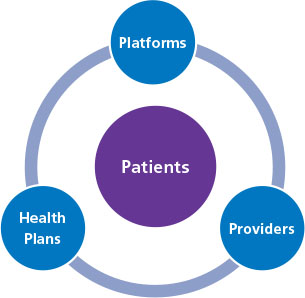
Because of this consensus, NCQA is developing telehealth standards for health plans, clinicians and platforms. We also:
- updated 40 HEDIS measures to incorporate appropriate use of telehealth,
- are incorporating telehealth into our nationally leading programs and new programs,
- have a dedicated cross-departmental team to stay abreast of rapidly developing telehealth issues and conduct research and policy assessments.
These efforts have led us to several key telehealth principles that we would like to share to guide its safe, effective and equitable integration into our healthcare system.
Healthcare’s Evolution into the Digital Age: Telehealth represents healthcare’s natural evolution into the digital age, and not a different type but another site or modality of care. As such, we should hold telehealth to the same standards of quality as other healthcare settings as much as feasible. We should also adapt, rather than reinvent, quality measures for telehealth. And telehealth, used appropriately, can be a critical tool in advancing well-coordinated, patient-centered, value-optimized healthcare.
Equity: COVID-19’s disproportionate impact on racial and ethnic minorities and other underserved populations underscores long-standing healthcare disparities that we must urgently address. Part of this includes taking rapid action to address substantial gaps in access to broadband technology, trust in that technology and digital literacy. This is essential for ensuring that, as healthcare moves into the digital age, we use telehealth to reduce rather than exacerbate disparities and must be a priority.
Care Coordination: Telehealth, again because of its digital nature, can improve care coordination under the right policies, but further fragment care without such policies. These policies include shared care plans and telehealth certification, as discussed above.
Lifting Outdated Telehealth Restrictions: Telehealth under COVID-19 proved that many old restrictions from when the technology was less sophisticated and use cases more limited are unwarranted. Going forward they should apply only if telehealth encounters do not meet appropriate standards of care or are necessary in specific situations. These include restrictions on:
- originating sites that prohibited telehealth, for example for patient homes,
- which clinicians can use telehealth and for what conditions,
- telehealth for patients who did not have a previous in-person relationship with a clinician, and
- telehealth care across state lines.
Old restrictions on tele-behavioral care in particular proved unwarranted, as a substantial increase in such care helped address added stressors during the pandemic. Given the great unmet need for behavioral care and that untreated behavioral issues drive costs by exacerbating both behavioral and physical conditions, we should embrace behavioral telehealth going forward.
Value-Based Care: Finally, and most important, value-based programs (VBP) best leverage telehealth. Old restrictions largely derived from fee for service (FFS) misuse concerns, not VBP where clinicians and other providers are free to utilize remote care to the degree that it meets patient needs and improves potential outcomes. Telehealth underscores the need to move even more rapidly to VBP.
We need consensus on appropriate telehealth standards. We need resources and effective approaches to address broadband, technology, trust and digital literacy gaps. We need effective policies for shared care plans that follow patients. And we need legislative and regulatory changes to permanently remove outdated telehealth restrictions and implement more targeted approaches.
So even as COVID-19 has generated so many new questions, we are certain on this: Telehealth must be an equitable and integral part of healthcare and meet standards for its safe, effective and appropriate use.





