Baton Rouge General Medical Center (BRGMC) did a review of their care management department to evaluate and identify structural and operational improvements. The reason for this review was to address growing hospital and physician concerns of patient delays in transitions for discharge. Nursing leadership was also concerned with the increasing number of patients being held in the emergency room awaiting a bed on the hospital unit. During the review process, it was identified that the care coordinators in the care management department at BRGMC should continue to serve as the single consistent resource for the patient, family, physicians and all the members of the care team; however, they should not have to complete all the logistical tasks required to implement a discharge plan. One of the main objectives of this process was to create a proactive care management team that could impact patient discharge outcomes and decrease discharge delays. These objectives correlate with the CMSA Standards of Practice for Case Management (2022) guiding principle to “foster safe and manageable navigation through the healthcare system to enhance the client’s timely access to services and achieve desired outcomes.”
BASELINE DATA
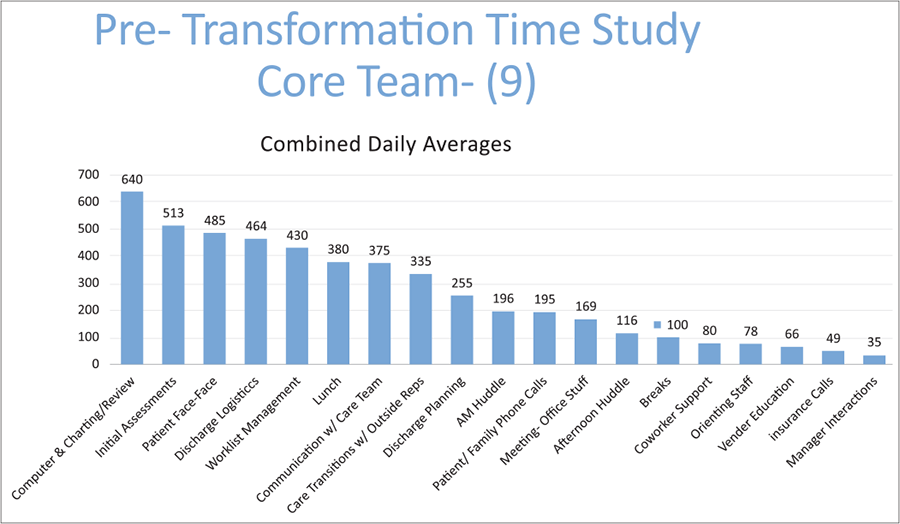
A time-study was completed by all care coordinators to identify tasks throughout their workday. This was completed by the care coordinators for a two-week period. Data was combined and separated into full-time staff tasks versus weekend/PRN staff tasks. Data showed that the full-time care coordination staff was spending 464 minutes per week and weekend/PRN staff were spending 273 minutes per weekend completing discharge logistics on patients; this was a per-staff average of 55 weekday minutes and 59 weekend minutes dedicated to discharge tasks. Discharge logistics were defined as tasks that anyone could complete, which did not need to be completed by a clinical staff member.
After the data was collected, a decision to create a post-acute resource center (PARC) was started. The PARC would be a centralized resource for all staff (physicians, residents, clinical team, nurses, care coordinators, etc.) to handle all post-acute needs that support discharge logistics without necessarily requiring care coordination intervention. The PARC would also be employed to help utilization review with notices that needed to be given to patients (Important Message from Medicare and the Medicare Outpatient Observation Notice).
The defined tasks included: transportation, DME, outpatient therapy referrals, post-acute referrals (home health, SNF, rehab, LTAC), arranging follow-up appointments, medication assistance and providing community resources.
A PARC steering committee was formed to handle all the logistics of designing and rolling out the implementation of the post-acute center. This committee included frontline care coordinators and key stakeholders who would interact with the post-acute center such as front-line nursing. Major components needed to achieve implementation success included a project plan, which included all the details needed from staff, location, building standard operating procedures and identifying key performance metrics. The PARC was staffed with trained non-clinical personnel who had healthcare experience with a minimum educational background of a high school degree. Staff were hired and trained initially to work five days a week and serve the internal care management department while they worked out processes and addressed any internal problems before a full go-live date was set for the entire health system. Once internal issues were addressed, such as turnaround time and communication logistics, additional staff were hired and trained to set up a seven-day-per-week schedule with staffed hours during peak discharge times to support hospital and emergency room patients across BRGMC.
SADIE HUTCHINSON, RN, DIRECTOR OF CASE MANAGEMENT FOR BATON ROUGE GENERAL MEDICAL CENTER.
CONSIDERATIONS DURING IMPLEMENTATION
One of the major considerations that the care coordinators (nurses and social workers) feared was how they were going to let go of these tasks to be handled by someone else. The care coordinators were unsure about how they would be interacting with patients and filling their day if they were not faxing and arranging transportation. A true cultural shift was required to get the care coordinators engaged in building a different relationship with their patients that was no longer about coordinating discharge tasks but about developing a strong patient assessment that proactively identified patient goals and barriers to discharge.
Another major consideration that occurred during the PARC rollout was learning how the care coordinators did not have a standardized workflow for planning and logistics of a discharge across the department. Although such items as “arranging home health” were loosely understood, the group of care coordinators varied on the details and documentation of their processes. This required the care coordinators to go back to redefining all workflows and developing a “best practice” guide for the department to ensure that training and implementation was held to standard. This made it clear which specific portions of the discharge plan would be conducted by the care coordinator, nursing and the post-acute coordinator. Standard operating procedures (SOPs) identified how items would be referred to the PARC, how staff would document and how each member of the care team would know when a task was completed.
During the implementation of the PARC, the steering team also had to overcome limited space and location logistics as well as various competing priorities of the healthcare organizations which pulled people away during the implementation process. Although these presented as delays in the project, the final objectives were achieved, just on a longer timetable than expected.
IMPROVING PATIENT OUTCOMES
The BRGMC care management department continues to monitor the success of the PARC to ensure they are meeting patient and organization expectations. Key metrics monitored are the number of referrals, where the referrals are coming from and the types of items requested. This helps ensure the program is meeting expectations for task completion and turnaround times. Since the implementation, the care coordinators on average saw a 50% reduction in time spent performing discharge logistics. From physician reporting and chart audits, documentation of case management screening and assessments improved from 67% of initials completed for appropriate patients, no later than five days from time of hospital admission to 82% post PARC implementation. Additionally, it should be noted that the staffing ratio maintained throughout this project was one care coordinator per 26-30 patients per assignment. Secondarily through this project, staff engagement increased as demonstrated by their pre- and post-transformation employee engagement scores. Avoidable days were also tracked throughout the project as an objective to decrease in relation to care coordination delays; however, true pre and post results could not be determined as it was found that staff were significantly underreporting avoidable days prior to project kickoff. This was due to lack of staff understanding related to avoidable day tracking importance and lack of leadership in the department prior to project transformation.
Today, the PARC at BRGMC is seen as an organizational success with any clinical staff member being able to place an order to the post-acute coordinators to facilitate transportation, make follow-up appointments and coordinate post-acute referrals. Post-acute coordinators can be seen interacting with nursing staff and in the hallways delivering notices to patients. This team has become an integral part of the discharge process for patients and continues to provide additional support to floor nursing in coordinating discharge tasks that do not require the use of the floor nurses’ time.
REFERENCE
CMSA Standards of Practice for Case Management, Revised 2022 Brentwood, TN.





