I sometimes wonder why patients are readmitted with the same diagnosis. Is it because they don’t follow the prescribed treatment plan, which can occur for a variety of reasons? Or did they not understand the discharge instructions?
Many times, patients just want to leave the hospital to go home, take a shower, eat the food their family cooks and sleep in their own bed. It is this rush that causes those beautiful written discharge instructions to be tossed into the patient’s belongings bag never to be seen again. But could there be more? My answer is a resounding yes. Here is a true story.
My 81-year-old father, who was very hard of hearing and had to have an ear amputation due to cancer, was hospitalized for exacerbation of heart failure. I received a phone call from him indicating he was ready to come home. When I entered his hospital room, the case manager was talking with him, and I saw his ever-present nodding of the head, indicating to most that he understood what was being said. The case manager appropriately asked me who I was, and of course the response was his daughter and his POA. I then asked Dad to let the case manager know it was fine for her to talk with me.
The case manager did a beautiful job of explaining the discharge plan, and with my dad shaking his head yes, she was under the impression he understood. However, when I asked him what she had just said, his response was he was going home tomorrow after my son picked him up and he was then going to come to my home. I explained that was not what was said. At the time, my son was states away in the Army and my dad lived in his own home. The case manager looked confused, and I explained to her the patient was extremely hard of hearing in his good ear and, as she could see, was missing the other. She asked why he was shaking his head yes and I told her it was because he was embarrassed to say he did not understand or could not hear.
A quick anatomy lesson: The outer ear, the ear lobe or pinna, was removed, which is the part that takes the sound and amplifies it into the ear canal. Without the pinna, hearing is much more difficult. Add this to the fact that this patient was already hard of hearing.
I asked the case manager to repeat the discharge plan, and she repeated it in the same tone and volume, and of course there was my dad shaking his head yes. The case manager never asked him to repeat what she said, a teach-back opportunity, and of course, he still did not understand what was being relayed.
Therefore, my case manager instincts kicked in and I explained to dad what the plan was. My voice was loud and in a neutral tone. The hospital case manager mentioned to me that I was yelling at him, and my response was no, I was speaking loudly so that he could hear me. I then asked him to repeat what I told him, and we were able to explain his discharge plan correctly. I also made sure he was able to communicate the plan moving forward, follow-up physician visits, etc., and he was able to do so.
The hospital case manager became disturbed, almost angry because she was under the impression I was yelling, and as she continued the discussion with my dad, she never increased her volume. Once again, I had to explain it to my dad at a louder volume so that he could not only hear but understand. The case manager then brought her manager into the picture.
When her manager arrived, the case manager explained she was attempting to give her patient discharge instructions but I kept interjecting. This was a great teaching opportunity for me.
So, I asked the case manager to please move forward with the next set of instructions, and of course it was at the same volume. Her manager could not see an issue, as my dad was once again shaking his head. The manager turned to me and asked what the problem was. So, I requested she ask my dad what was just said to him. As you guessed, it was nothing that was just mentioned. The manager looked perplexed and confused. Now it was my time.
The first question I asked the manager was, what did she notice about my dad’s appearance, and of course she mentioned the missing ear. The next question was, did she think an 81-year-old with a missing ear and hard of hearing documented on the chart could understand what was being said in hushed tones, and she said no but he kept shaking his head yes. I explained that he does this because of embarrassment to mention he did not hear what was said or may not have understood what was said. The last question was, do her case managers employ the teach-back method, and again, there was a confused look on her face. (I have to admit this was when I was starting to lose my patience and had to bite my tongue to not say what I really wanted to say.) So, I once again explained to Dad what was said in a loud volume. I then asked him to explain what I just said and to tell me what it meant, and he was able to do so without issues. The manager then had that “ah-ha” look on her face.
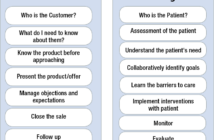
Now was my teaching opportunity. I explained my role as an independent case manager as well as my extensive involvement in case management organizations. Now her interest was really high. So, I continued. We discussed teach-back methods and why they were important; motivation interviewing was explained and how it can be very helpful when discussing issues with our patients. She opened her laptop and we reviewed many links where she could seek assistance in teaching her staff on proper discharge planning.
We then discussed some possible reasons discharge planning may not be done correctly. Is it because of the hospital being short-staffed, is it the case management model they employ and/or is it the lack of education within their department? It was a great discussion, and when Dad was admitted a few months later, it was fabulous to see the change in the case management staff, and I let that manager know.
She took the time to visit me while I was there and stated she had incorporated lunch and learns using some of the resources that were available and even noticed their patient satisfaction scores had improved and their readmission rate had started to decrease!
I know other people who have had similar experiences. The discharge planner did not take the time to truly investigate what was needed, did not talk with the patient and/or family and did not question the physicians if something was not understood.
It is because of my dad as well as other stories that I have heard from other case managers who have had loved ones in the hospital that I challenge all case managers who perform discharge planning, no matter the setting, to take a look at your processes. If you were the patient or family, could you understand what was being said or done? Could you give instructions in laymen’s terms? In other words, what can you do better?
Case managers play such a pivotal role with our patients that we cannot afford to become lax in our processes, ethics, standards or practice. We must always strive to do and be better.